Reports
Health
Wellness
For years, diets called for the elimination of fats, urging us to move towards low-fat alternatives. While, like any other nutrient, overdoing fats can lead to weight gain, cutting out dietary fats need not necessarily result in weight loss. Replacing bad fats (trans fats, saturated fats) with good fats (mono and poly-unsaturated fats) comes with benefits that extend beyond weight loss. This article covers everything there is to know about incorporating monounsaturated fats in your diet.
Fats are an important component of any meal as they help in absorbing fat-soluble vitamins and minerals.
They also store energy within the body, protect vital organs, and help in muscle movement.
Fats are chains of carbon and hydrogen, and depending on the length of these chains and the arrangement of these atoms, they are classified into different types of fats.
The “mono” in monounsaturated fats represents the single double bond that is found in its chemical structure.
Owing to this chemical structure, monounsaturated fats are often liquid at room temperature.
Anthropologists claim that the diet of early humans was more similar to that of modern chimpanzees. They consumed fruits, vegetables, leaves, flowers, and meat. It is believed that meat was first consumed about 2.6 million years ago.
However, our early ancestors engaged in scavenging food rather than hunting. They consumed the edible portions of flesh that were left behind by the predator. Jesicca Thompson, an anthropologist from Yale University, says that the early humans consumed bone marrow stuck in between the bones of the dead animal rather than the “meat.” The marrows are rich in fat content. Thompson claims that it was around this time that humans started adding fat-rich food to their diet.
Modern-day diet has monounsaturated fats in vegetable and seed oils. A study confirmed that the first use of vegetable oil, particularly olive oil, was seen around 8000 years ago in the Middle East. But it was in the 1600s when people started making oil from vegetables.
The 1800s saw the widespread use of vegetable oil as the commonly used whale oil became expensive. In the process of making affordable soaps using cottonseed oil, two industrialists in Cincinnati took the opportunity to introduce it in the food industry. In a few years, animal fats were replaced by vegetable cooking oils, and we can still find them in our kitchens today.
Studies observed that people from the Middle East or the Mediterranean countries had a lower risk of heart diseases, despite consuming a fat-rich diet. Further investigation showed that their diet included olive oil and other seed oils as their main source of fat and not animal fat. This could mean that the health benefits come from unsaturated fats rather than saturated fats from animals.
A study consisting of around 840,000 adults aged 4-30 years found that the consumption of monounsaturated fats reduced the risk of heart disease by 12%, compared to the control group (little to no monounsaturated fats consumption)
Monounsaturated fats improve overall health by:
Sources of monounsaturated fats are olive oil, peanut oil, avocados, nuts, safflower, and sunflower oils.
Weight gain is caused when the calories consumed are greater than the calories burnt.
All fats provide the same amount of energy, which is about nine calories per gram.
Based on your lifestyle and your basal metabolic rate, including the right amount of fat in your diet, can help with weight management.
Even though weight gain/loss is a simple equation of calories in and out, the quality of the food you eat as part of your diet is very important.Some studies have shown that if calorie intake remains the same, diets high in MUFAs lead to weight loss and could even be more effective than a high-carb diet.
It is recommended to use monounsaturated fats as a replacement to saturated or trans-fats as much as possible.
The 2015 Dietary Guidelines for Americans suggest that fats should be limited to 25 to 30% of the total daily calories; this includes all types of fats.
This gene is involved in the control of fat metabolism (break down) and insulin sensitivity (how well your body responds to insulin) in the body.
Changes in this gene directly affect anti-diabetic, anti-atherogenic (preventing fatty deposit formation), and anti-inflammatory activities.
The gene codes for a protein called the adiponectin, that is involved in aids fatty acid breakdown. Higher the adiponectin levels, more efficient the fatty acid breakdown.
Decreased adiponectin levels are thought to play a central role in obesity and type 2 diabetes.
Changes in lifestyle, such as incorporating exercise and a following balanced diet, that result in weight loss, can lead to an increase in adiponectin concentration and increase insulin sensitivity.
A study found that a variation rs17300539 in the ADIPOQ gene can lead to a difference in blood adiponectin levels.
Individuals with a G allele have lower blood adiponectin levels when compared to those with an A allele. Carriers of the A allele (AA/AG), therefore, had lower weight, BMI, waist, and hip circumferences.
While considering the monounsaturated fats intake of greater than 13% of the total energy intake, the A allele carriers had a considerably lower BMI compared to GG carriers.
This shows a relationship between the effect of a gene on monounsaturated fats intake and weight.
NR1D1, also known as Rev-ErbA alpha, is present in the liver, skeletal muscles, adipose (fat) tissues, and the brain in mammals.
Adipogenesis is the process by which adipocytes, or fat cells are formed.
Rev-ErbA alpha includes adipogenesis and could be a potential target for novel anti-obesity treatments.
A study analyzed the association between NR1D1, monounsaturated fats intake, and weight in North American and Mediterranean populations.
People with the AA and AG types had a lower waist circumference and a decreased risk for obesity than people with the GG type.
The A allele occurrence was also significantly low in the ‘abdominally obese’ group.
There was also a significant interaction for obesity with NR1D1 and monounsaturated fats intake in the Mediterranean population.
Individuals with the A allele had higher protection against obesity with diets rich in monounsaturated fats. (>55% of total fat).
PPARG is a gene predominantly present in adipose tissue. It plays a role in adipocyte differentiation (converting one type of cell to another), regulating glucose levels, and insulin signal transduction (communication between two cells).
A change in this gene has been studied to play a role in increased sensitivity to insulin and a more favorable lipid profile.
A study recruited overweight subjects between the ages of 20-65 years in southeastern Spain.
They analyzed the subjects as they underwent a treatment program for obesity.
This included analyzing the diets and the number of calories expended during exercise.
They found a gene-diet interaction between PPARG and monounsaturated fats intake.
People who had the G allele (CG/GG) were significantly less obese than those with the C allele (CC) - when monounsaturated fats intake was high (>56% of total fat).
This difference disappeared in low monounsaturated fats diets.
Overall, in each case, diets with high monounsaturated fats intake (>55% of total fat) resulted in a greater weight loss in individuals.
Most foods have a combination of all types of fats. Foods and oils that have a higher percentage of MUFA are:
Fats are a necessary component in a balanced diet. However, not all types of fats are healthy. While saturated fats are the ‘bad fats,’ the unsaturated fats are ‘good fats.’ Monounsaturated fats or MUFAs are fats joined by a single bond. They help reduce the risk of health conditions like diabetes and cancer. They also enhance insulin sensitivity and, therefore, play a role in weight management. Several genes ADIPOQ, NR1D1, and PPARG, mediate how your body responded to MUFAs in terms of weight gain. People with certain types of these genes tend to benefit more from MUFA consumption in terms of weight loss and can include more MUFA-rich foods in their diets. Some food sources of MUFAs include avocados, olive oil, peanuts, and eggs. Even though MUFAs are present in certain animal sources like red meat, their benefits are negated by the saturated fats in them.
Our body is fueled everyday by different nutrients – some that are required in larger quantities while others in lesser, and few in traces amounts. Some nutrients form structural components of our cells whereas, there are others that participate or regulate various functions and processes in the body. One such trace mineral, and an essential one too, is copper.
Our body needs minerals for various physiological processes.
While some minerals are needed in larger quantities like sodium, calcium, and potassium, some like copper are essential trace minerals that are vital for survival.
Copper is found in all body cells and plays an important role in the formation of blood vessels, maintenance of the nervous, and the immune system.
Our body has about 2 mg of copper per kilogram of body mass.
Though copper is found in all parts of the body, organs like the liver, kidney, heart, and the brain have it in higher quantities.
As mentioned earlier, our body needs copper for plenty of activities. These include:
Intake of less than the Required Dietary Allowance (RDA) of copper can lead to copper deficiency whereas, taking in more than the RDA can lead to copper toxicity, both of which can be harmful.
For adolescents and adults, the RDA is about 900 mcg per day.
Any intake above 10,000 mcg or 10 mg per day can be toxic.
The copper requirement of the body changes with age, gender, and conditions like pregnancy.
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| 0-12 months | 200 mcg | 200 mcg | ||
| 1-3 years | 340 mcg | 340 mcg | ||
| 4-8 years | 440 mcg | 440 mcg | ||
| 9-13 years | 700 mcg | 700 mcg | ||
| 14-18 years | 890 mcg | 890 mcg | 1000mcg | 1000 mcg |
| 19+ years | 900 mcg | 900 mcg | 1300 mcg | 1300 mcg |
Copper deficiency can occur due to diet, nutritional deficiencies, or digestive issues resulting from surgeries or other conditions.
These are called acquired copper deficiencies.
Another type of copper deficiency is inherited copper deficiency that is genetic in origin.
Surgeries like bariatric surgery, gastrectomy, upper GI tract surgery, and other stomach surgeries result in copper deficiency.
Inherited copper deficiency is rare and affects one in every 1,00,000 births.
The gene causing this condition is inherited in an X-linked recessive manner and runs in families.
The SELENBP1 is located on chromosome 1 and is a part of the selenium-binding protein family.
Selenium is an essential mineral and is known for its anticarcinogenic properties and a deficiency of it can result in neurologic diseases.
The protein encoded by the SELENBP1 gene is said to play a selenium-dependent role a ubiquitination/deubiquitination-mediated protein degradation.
One of the phenotypes for the SELENNP1 gene is serum copper measurement.
The presence of the G allele in this SNP causes a decreased absorption of copper resulting in an increased risk of developing a copper deficiency.
The SMIM1 gene or Small Integral Member Protein 1 is located on chromosome 1 and codes for a small, conserved protein that takes in part in the formation of red blood cells.
The A allele of the SNP rs1175550 is associated with serum copper measurement.
The main problem with copper deficiency is that it is hard to diagnose as its symptoms are very similar to other nutritional deficiencies such as vitamin B12 deficiency.
Since low copper levels in the body can affect a person’s immunity, it is important to identify it in time.
Clinical symptoms of copper deficiency include:
Copper deficiency can also be recognized hematologically as it presents with a triad of anemia, neutropenia, and thrombocytopenia (rare).
Copper deficiency is usually not the first thing that is diagnosed when one presents with symptoms as many nutritional deficiencies present with similar clinical symptoms.
However, your doctor may suspect copper deficiency if you have a history of any of the following:
If your doctor suspects a copper deficiency, he/she may order a blood test for detecting plasma copper levels.
However, one must note that this is not a conclusive test for copper deficiency as many other factors can cause a false elevation of blood copper levels.
The first step in the treatment of copper deficiency is identifying the cause and removing or treating it.
For example, if the copper deficiency is due to excess zinc supplements, your doctor will reduce the zinc supplements to allow more absorption of copper.
Many a time, doctors prescribe copper supplements to make up for the deficiency of the mineral.
Common copper supplements include copper sulfate, copper gluconate, and copper chloride.
It can take about 4 to 12 weeks to treat a copper deficiency.
Taking 2 mg of copper per day can help restore normal copper levels in a deficient individual.
However, the exact dosage is determined by a doctor after evaluating other health and lifestyle factors.
In the case of individuals who cannot take oral copper supplements, they may be put on IV copper treatment.
Along with copper supplements, consuming copper-rich foods can really help.
Copper is an essential mineral for the body but it is also a trace mineral which means that our body needs a very little amount of copper to function.
However, many people suffer from a deficiency of this mineral that can result in complications over a period of time.
Some people who require copper supplements include:
However, care must be taken to consult with your doctor before taking copper supplements as copper toxicity can be as harmful to the body as copper deficiency.
Apart from this, people who have had surgery such as bariatric surgery, gastrectomy, or those who suffer from GI tract diseases such as IBS, celiac disease, etc., also need supplements as they are more likely to have copper deficiency due to the poor absorption.
There are certain rules to follow when taking copper supplements. We know that zinc interferes with copper supplements and so, avoid taking both zinc and copper supplements at the same time.
Fix two different times for both supplements and stick to these times every day.
Ideally, take your copper supplement at least two hours after taking your zinc supplements for maximum absorption.
Copper supplements can cause stomach irritation and acidity, and hence, copper supplements can be taken with meals can help reduce irritation.
Many people who take antacids may need higher dosages of copper supplements as antacids interfere with the absorption of copper.
Copper supplements can cause side effects and the common ones are:
There are symptoms of overdose that one must watch out for and avoid:-
Apart from supplements, diet plays an important role in restoring normal copper levels in the body.
To treat copper deficiency and maintain optimum copper levels in the body, some copper-rich foods that you can include in your diet are:
Upload your raw data to Xcode Life for insights into 700+ health-related traits!
https://ods.od.nih.gov/factsheets/Copper-HealthProfessional/#en3
https://www.genecards.org/cgi-bin/carddisp.pl?gene=SELENBP1
https://www.snpedia.com/index.php/Rs2769264
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3766178/
https://www.genecards.org/cgi-bin/carddisp.pl?gene=SMIM1&keywords=SMIM1
Ever wondered how going off carbs for a couple of days almost always shows instant results? Thank all the glycogen stored in your body. But some people have trouble storing this entity as we do, disrupting their chance to live a typical life. Let’s peak into what actually happens with Glycogen Storage Disease.
Metabolism is a biological process that breaks down the food we eat and provides energy to keep us alive.
In some cases, different key stakeholders in this process fail to fulfill their duty.
There is a spectrum of conditions that fall under the umbrella of Glycogen Storage Disease (GSD), which cause such trouble.
Since it did not have any popular awareness challenge go viral (bring back the ice buckets!) and fortunately is a rare condition, it hasn’t had too much light thrown on it.
According to the reports, the incidence rates appear to be 1 in 100,000.
As the symptoms set out at an early age, Glycogen Storage Disease appears to affect the little ones more than the adults.

Our body uses glycogen, a complex sugar compound, as a fundamental storing unit of energy. Metabolizing glycogen, to break it down into glucose, provides the instant energy we need. As we need to conserve some of this energy, these glucose molecules are combined back into glycogen. This is used as a reservoir to tap into when there is a lack of energy supply. Different parts of the muscles and the liver act as storage units for glycogen.
For this process to take place, some special proteins called enzymes (biocatalysts) aid the formation and deformation of glycogen.
When these enzymes don't function optimally, it leads to a spectrum of diseases.
This could lead to a range of different symptoms depending on the type of diseases.
The types are classified based on the enzyme which is at fault. It starts from GSD1 and runs up until GSD 15.
The types 1 to 4 cover almost 90% of the reported cases, with sub-type of GSD1 - GSD 1a, aka Von Gierke Disease being most common.
As the condition affects the necessity of food metabolism, symptoms start to show 3 to 4 months after birth.
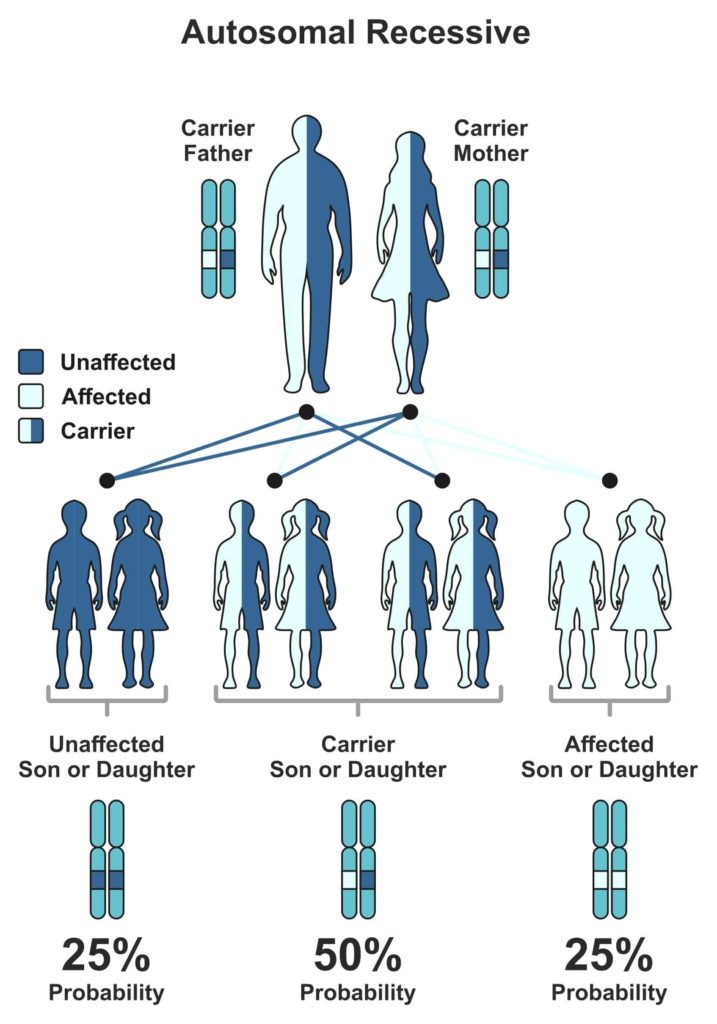
The cause of Glycogen Storage Disease is genetic.
The gene that is responsible for the malfunction of the enzyme can pass on from the parent generation to the next, making it hereditary.
But the child will express symptoms of the associated GSD, only when both parents possess a defective gene.
Every human gets their 23 chromosomes from each parent.
Genes that are subunits to chromosomes have one trait, which is dominant and other recessive (some exceptions, of course).
The level of expression marks the difference between them.
Now, for the expression of a recessive trait, both parents must pass on their recessive versions of traits.
The Mendelian world calls this an autosomal recessive condition.
A random process selects the gene to be passed down to the next generation.
In the case of autosomal recessive conditions, there is a 25% chance of occurrence.
If just one parent passes it on, then the child will remain healthy but acts as a carrier of the gene.
Carriers could potentially pass it on to the coming generations.
We obtain glucose from the diet we eat.
Glycogenin is an enzyme that is responsible for cutting down this glucose into short fragments.
Another enzyme, glycogen synthase, helps in the conversion of glucose into Glycogen.
Now, some branching enzymes add branches to Glycogen, which the liver then stores as a reservoir of energy.
When we fast or there is a need for muscle contraction, the body taps into the said reservoir.
The process of breakdown involves four enzymes.
Glycogen Phosphorylase and glycogen debranching enzymes help in unraveling the molecule to release glucose and expend energy.
Another method of breaking it down involves enzymes such as a-glucosidase and Glucose-6-phosphatase.
Every action in our body is instructed by the beautifully wound helix, DNA.
As these enzymes correspond to specific genes, any defect in this gene will directly translate into the enzyme’s action.
Take the example of the most common type of GSD - GSD type 1a.
One of the enzyme genes involved in breaking down glycogen is Glucose-6-phosphatase. G6PC and SLC37A4 genes code for this enzyme.
As genes code for proteins and proteins like enzymes carry out the function, an error in the gene structure or function will lead to a collapse of the entire system.
A good analogy would be a loose brick in a building that could make it fall into pieces. Geneticists call these errors, mutations. As these ‘errors’ have been major contributors in the history of evolution, they have been beneficial in many ways.
Unfortunately, not in the case of Glycogen Storage Diseases.
So, when there is a mutation in this gene, glucose-6-phosphatase does not play its role and leads to the build-up of Glycogen and fat.
We know, too much of anything is toxic. Hence, the accumulation of Glycogen and fat hinders the function of organs like liver and kidney.
In the case of type 3 Cori disease/Forbes disease, a distinct part of the gene, called Exon3, carries two mutations that cause the debranching enzyme to malfunction.
As a debranching enzyme is responsible for the decomposition of Glycogen, it leads to toxic accumulation.
Andersen disease (type 4) affects the GBE1 gene that codes for glycogen branching enzyme leading to large amounts of abnormal Glycogen accumulated, causing severe conditions like liver cirrhosis, which is ‘doctor’ for scarring.
Types 1, 3, and 4 are far more common in comparison to other types.
Most often, all different types have a combination of some common symptoms in varying intensities.
As the age of onset is rather young in the case of Glycogen Storage Diseases, doctors generally ask the parents about symptoms showcased by their child and call for relevant tests.
Blood tests and MRI/ultrasound scans are routine. In some cases, a biopsy of a suspected organ might be required for confirmatory diagnosis.
Genetic testing has evolved over time and is performed to confirm the diagnosis.
This is extremely helpful in the case of couples who have observed a family history of Glycogen Storage Disease.
Seeking genetic counseling before planning a family will help provide a clearer picture of the chance of occurrence in their case.
Carrier testing for at-risk family members and prenatal diagnosis have led to significant changes in family planning.
The treatment options are specific to the type of GSD diagnosed with the patient.
Generally, it includes major dietary restrictions.
Uncooked corn starch can be a good feed to children over two years of age, as corn starch can promise a slow release of glucose.
This is fed in small portions throughout the day.
For type 1, elimination of food which is high in lactose and fructose is advised (that's pretty much everything tasty, from mozzarella to maple syrup).
Allopurinol is prescribed if there is a risk of kidney stones or gout, as it reduces the levels of uric acid in the blood.
Some extreme cases like the type 4 of GSD could require liver transplant depending on the extent of the condition.
When the patient is prone to frequent muscle cramps during exercise, a high protein diet is advised.
In some cases, the intake of glucose and fructose is advised. And of course, as their muscles are now more susceptible to damage, over-exhausting the body is a big No-No.
Unfortunately, prevention is barely an option.
As this is a genetic condition, the only way of prevention is to ‘not pass on the genes’.
Parents can seek genetic counseling to check if both carry the defective gene as it takes two to tango in this case.
But we have come a long way with the prognosis of the condition.
The unawareness of the disease’s details led medical researchers to believe GSD to be a fatal condition until the early ’70s.
People now live long and normal lives with significant dietary shifts.
This barely seems like a change in the millennial world of Keto and Atkins!
Speaking of Keto and Atkins, Glycogen is the secret quarterback in the low-carb diet game.
Glycogen storage and weight loss have a strange love story.
A typical healthy liver in an individual can hold up to 400 grams of glycogen and muscle cells, about 100 grams.
As glycogen and water co-exist in a 1:3 ratio, there are 3 grams of water present for every gram of glycogen.
This is the real reason behind the initial weight loss observed when any sort of low-carb diet is practiced.
It would rather be ideal for comparing body fat percentage or keeping track of monthly weight changes, for getting a better measure of body change as opposed to this initial quick loss of weight.
The body stores about 1500-2000 calories of Glycogen typically.
With a low-carb diet, the body uses this up and has little or no reservoir of energy. Possibly dehydrated.
This can lead to a constant state of fatigue in some extreme cases that could potentially damage the liver as it would be exposed to undue stress.
So we should be cautious when we make such lifestyle changes and always seek professional guidance.
In the case of sportsmen, a low-carb diet could lead to quick use of the stored Glycogen, especially the ones stored in the muscles.
This leads to a case of muscle fatigue and, in extreme cases, will lead to a phenomenon known as “hitting the wall”. Glycogen is also brain food.
So severe lack of Glycogen leads to cognitive symptoms like confusion, disorientation when you have a “bonk” during exercise.
Though there is cutting current edge research to discover new enzyme replacement therapies and gene therapies, this spectrum of diseases affects many lives.
But once again, we are hopeful that genomics will save the day!
Upload your DNA raw data to Xcode Life for insights into 700+ health-related traits
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4146814/ - Ozen H. (2007). Glycogen storage diseases: new perspectives. World journal of gastroenterology, 13(18), 2541–2553. https://doi.org/10.3748/wjg.v13.i18.2541
https://www.tandfonline.com/doi/full/10.3109/01913123.2011.601404 - Hicks J, Wartchow E, Mierau G. Glycogen storage diseases: a brief review and update on clinical features, genetic abnormalities, pathologic features, and treatment. Ultrastruct Pathol. 2011;35(5):183‐196. doi:10.3109/01913123.2011.601404
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(04)16986-9/fulltext Astrup, A., Meinert Larsen, T., & Harper, A. (2004). Atkins and other low-carbohydrate diets: hoax or an effective tool for weight loss?. Lancet (London, England), 364(9437), 897–899. https://doi.org/10.1016/S0140-6736(04)16986-9
https://onlinelibrary.wiley.com/doi/abs/10.1038/icb.2015.109 - Gleeson M. (2016). Immunological aspects of sport nutrition. Immunology and cell biology, 94(2), 117–123. https://doi.org/10.1038/icb.2015.109
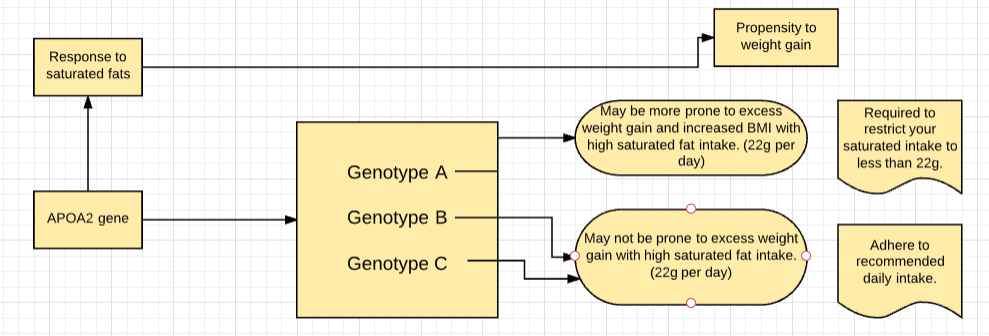
Our genes are a template for how our bodies work. Most people on keto diets tend to consume a high amount of saturated fats. The diet works only when the stored fat is properly broken down and used for energy. Certain variants of the APOA2 gene tend to interfere with this saturated fats metabolism and hence, carriers of such variants may not get the desired benefit from this diet.
There seems to be an endless debate about whether saturated fats are good or bad for your health.
The truth is, all of us need a little bit of fat for some body functions like hormone production or maintenance of cell integrity.
But, what is considered 'too much' for your body is determined by certain gene variants you carry.
Let's explore this concept with a diet that's been constantly gaining popularity for weight loss and prevention and treatment of certain health conditions:
The basis of this diet is ketosis, which refers to the metabolic process in which the body converts stored fats into energy, releasing ketones in the process.
Hence, the conventional keto diet, which calls for high consumption of fats may work only if the stored fat is metabolized efficiently.
Several genes contribute to how your body reacts to saturated fats.
APOA2 gene is one of them that determines how well you tolerate saturated fats and how well you can transport cholesterol.
Depending on the variant of this gene you carry, you may need to modify the keto diet a little bit, in order to maximize its benefits to your body.
From the evolutionary perspective, certain human societies, such as those in the colder northern regions are likely to have subsisted on the large intake of fats for hundreds of generations.
As a result, they could have developed adaptations that enable them to metabolize this macro ingredient in food quite efficiently.
If you have inherited those genes, then your body is better able to cope with fats intake.
APOA2 gene produces a protein apolipoprotein -II, which plays a role in fat metabolism and obesity.
Individuals with the sensitive variant of this gene are more prone to increased BMI (6.8 times greater BMI), waist circumference, and body weight in response to high levels of saturated fat (more than 22g of saturated fats per day).
This was an observation in comparison to the people with the non-sensitive variant of the gene consuming the same amount of saturated fats.
It is vital for the carriers of the sensitive variant to limit their saturated fat intake.
However, there was no difference among individuals with both versions, in terms of weight and BMI when saturated fat intake was low (less than 22g per day).
One possible mechanism that could help explain the above gene-diet interactions is that, the sensitive variant of this gene produces lower levels of the protein, APOA2 (regulates the satiety response), resulting in low satiety and greater appetite among individuals with higher saturated fat intake.
This appetite may preferably be for foods rich in saturated fat and this higher fat intake would lead to greater weight.
Other genes like FTO, PPARG also impact the metabolism of saturated fats.
Carrying even 2-3 variants that affect saturated fats metabolism can pose a challenge to cholesterol control and weight loss.
It is thus vital for such individuals to alter their diet with lesser intake of saturated fatty acids.
Replacing saturated fatty acids with monounsaturated fatty acids (MUFA) and poly-unsaturated fatty acids can be a good start.
Sources of MUFA
Sources of PUFA
Upload your DNA raw data to Xcode Life to know your genetic variants for saturated fat metabolism.
Carbohydrates are one of the main classes of food. It is the main source of energy for the body. They are a group of organic compounds present in the form of food in cellulose, starch, and sugar. They are called carbohydrates, as they contain hydrogen and oxygen in the same ratio as water (2:1). These are then broken down to release energy.
Due to the association of carbohydrates with weight gain, the carbs may disguise as an enemy to a healthy diet. However, the right kind of carbs in the right amounts can definitely earn a rightful place in your diet.
A healthy weight is an important element of good health. The amount of food you eat and what you eat is important for maintaining a healthy weight.
For years, there was a myth that a low-carb diet is the best way to lose weight, but a growing body of evidence suggests otherwise.
Carbs are sub-divided into three categories depending on the number of sugars present and the nature of the chemical bonds between them.
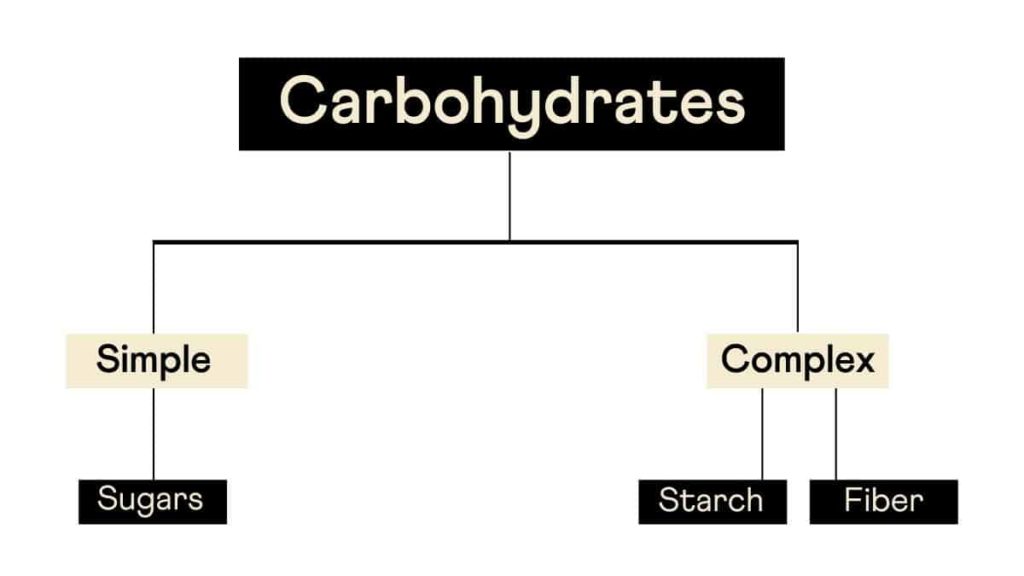
Although this is the conventional way of classifying carbs, a more pragmatic approach would be to classify them as refined and whole carbs.
Whole carbs include vegetables, legumes, whole fruits, and grains, which are unprocessed and thus have their nutrient content intact.
The stripping of nutrients in refined carbs as a part of processing makes them count as 'empty calories.'
This removal of the nutrients results in rapid absorption and metabolism of these carbohydrates.
This results in spiked sugar levels and unstable energy levels, the latter of which causes “sugar rush” after consuming sugar-rich foods.
The refined or the sugary carbs are simple carbohydrates that the body quickly absorbs.
Their metabolism occurs rapidly, which results in major swings in the blood glucose levels. This induces hormonal and metabolic changes that can promote overeating.
Not all carbohydrates are bad for health.
Unprocessed carbs that are present in vegetables, fruits, and grains are healthy.
Studies reveal that these improve metabolization and help in weight loss.
Another class of carbs, the processed ones, are unhealthy because they lose the fiber during processing and contain no essential nutrients.
Examples of these include white bread, white rice, and the like.
Intake of foods containing processed carbs can result in weight gain and increased risk of type 2 diabetes.
Studies show that high unprocessed carbs in the diet can lead to a craving for more carbs, and people tend to get caught in the vicious cycle.
Thus, making changes to your diet by including more of unprocessed carbs can be a healthy choice.
Studies have shown that there is a link between genetic factors and dietary factors such as weight loss, weight gain, obesity.
Nearly 70% of the world population carries the gene for obesity. This explains why obesity is growing rapidly around the world.
However, people can reverse this gene's effect by exercising and including more protein in their diet.
A study has found an association between the FTO gene and the intake of carbohydrates.
The individuals with the A variant were found to have a higher risk of obesity than ones with the CC wild type.
The FTO gene has a negative association with over-eating.
About 23% of the global population carries a variant in the AMY1 gene, which shows an association with low copy numbers of the gene and reduced ability to digest starch.
70% of people from agricultural populations have an AMY1 copy number variant, which shows an association with better starch digestion and lower risk of obesity when compared to 37% of non-agricultural populations.
The conventional diet plans and workout regimes architected for weight loss need not help everyone achieve their desired goals.
There is a multitude of factors that influence weight loss, including a person’s lifestyle, genetic makeup, and the environment.
Your genes can influence how you metabolize the nutrients you get from your diet. This directly has a role to play in weight gain/loss.
For instance, some people may possess a genetic variant that aids in the faster metabolization of carbohydrates, while others may carry a variant that will help in faster break-down of saturated fats.
You can leverage such genetic information to adopt a practical and personalized weight loss plan.
While genetic tests may not lay out the A-Z of weight loss, it certainly helps you pin the right path for your weight loss journey.
Upload your DNA raw data to Xcode Life for insights into 700+ health-related traits
CYP1A2 codes for the production of 21-hydroxylase, which is part of the cytochrome P450 family of enzymes.
This family of enzymes is quite important as it is a part of many processes, that include breaking down drugs, production of cholesterol, hormones, and fats.
The adrenal glands secrete the enzyme, 21-hydroxylase.
Situated on the top of the kidneys, the adrenal glands also produce hormones like epinephrine and cortisol.
Incidentally, 21-hydroxylase plays a role in the production of cortisol and another hormone named aldosterone.
Cortisol is a stress-related hormone and plays a role in protecting the body from stress, as well as reducing inflammation.
Cortisol also helps in maintaining blood sugar levels.
Aldosterone, also known as the salt-retaining hormone, regulates the amount of salt retained in the kidneys.
This has a direct consequence on blood pressure, as well as fluid retention in the body.
There seems to be an interesting trend in the activity of the CYP1A2 gene and caffeine intake.
The consequence of being a “rapid” or a “slow” metabolizer of caffeine can have effects on an individual’s cardiovascular health.
This article explains the wide-ranging effects of this gene, caffeine intake, cardiovascular health, hypertension, and even pregnancy!
In the body, CYP1A2 accounts for around 95% of caffeine metabolism.
The enzyme efficiency varies between individuals.
A homozygous, that is, AA genotype represents individuals that can rapidly metabolize caffeine.
Some individuals have a mutation in this locus and thus have the AC genotype.
These individuals are “slow” caffeine metabolizers.
There seems to be a link between CYP1A2, the incidence of myocardial infarction (MI), and coffee intake.
The positive effects of coffee include lowering a feeling of tiredness and increasing alertness; however, it can also narrow the blood vessels.
This increases blood pressure and could lead to cardiovascular disease risk.
Rapid metabolizers of coffee have the AA genotype and may unravel the protective effects of caffeine in the system.
However, the individuals that are slow metabolizers have a higher risk of MI.
This suggests that the intake of caffeine has some role in this association.
Yet another study associated DNA damage due to mutagens found in tobacco smoking could contribute to MI.
The study included participants who were genotyped at the CYP1A2 gene.
They found a group of ‘highly inducible’ subjects that had a CYP1A2*1A/*1A genotype.
These individuals have a greater risk for MI, independent of their smoking status.
This also means that there is some intermediary substrate that the CYP1A2 gene decomposes, and if this gene has a mutation, it could lead to a higher risk of MI.
In a study conducted on 2014 people, people who were slow metabolizers of caffeine (C variant) and who consumed more than 3 cups of coffee per day had an association with increased risk for myocardial infarction.
In a similar study on 513 people, increased intake of coffee, among slow metabolizers, has an association with an increased risk for hypertension.
Smoking is capable of inducing the CYP1A2 enzyme. Smokers exhibit increased activity of this enzyme.
In a study conducted on 16719 people, people with the A variant, and who were non-smokers, were 35% less likely to be hypertensive than people with the C variant.
In the same study, CYP1A2 activity had a negative association with blood pressure among ex-smokers.
But for people who were still smoking, the same gene expressed an association with increased blood pressure.
The gene CYP1A2 also has an association with caffeine metabolism and smoking.
A study aimed to tie these concepts together to find the relationship between this gene and blood pressure (BP).
The main measurements of the study were caffeine intake, BP, and the activity of the CYP1A2 gene.
In non-smokers, CYP1A2 variants (having either a CC, AC, or AA genotype) were associated with hypertension.
Higher CYP1A2 activity was associated with people who quit smoking and had lower BP compared to the rest but had a higher BP while smoking.
In non-smokers, CYP1A2 variants (having either a CC, AC or AA genotype) were associated with high caffeine intake, and also had low BP.
This means that caffeine intake plays some role in protecting non-smokers from hypertension, by inducing CYP1A2.
The intake of caffeine during pregnancy has an association with the risk of reduced fetal growth.
High caffeine intake shows a link to decreased birth weight.
The babies are also at risk of being too small during the time of pregnancy.
This was also observed in a study conducted on 415 Japanese women.
Women with the A variant who drank more than 300 mg of coffee per day were shown to be at an increased risk of giving birth to babies with low birth weight.
In conclusion, there are a lot of effects that the CYP1A2 gene has on the body. Many studies, as noted above, seem to link the activity of this gene to caffeine intake.
A variant at the CYP1A2 gene can determine whether an individual is a fast or slow metabolizer of caffeine, and this has some effect on the blood pressure and cardiovascular health of an individual.
The gene also plays a role in regulating an infant’s weight during the pregnancy of a woman, and this has a link with caffeine intake. It is thus interesting to analyze the effect of the variants of the CYP1A2 gene on an individual, based on their caffeine intake.
Upload it to Xcode Life to know about your CYP1A2 caffeine metabolism and caffeine sensitivity variants.
Well, you’ve heard it umpteen times that you are what you eat. You are probably gearing up already to redesign your food chart to throw in a few healthy choices based on nutritionists' recommendations.
In that case, you must be familiar with the term “antioxidants” – the magical word in the lexicon of health and nutrition that has become a synonym of power-houses of nutrients.
After all, who wouldn’t want to look perennially young, be energetic, and free of ailments! Though such a proposition may sound a fantastic probability, you can turn it into a possibility by opting for a sensible diet plan that includes foods rich in antioxidants.

Antioxidants are naturally occurring chemicals in foods that help to counter the detrimental effects of oxygen free radicals, which form during normal metabolism.
External factors like pollution, ultra-violet radiation, and X-rays also produce free radicals that affect our system. Free radicals are deprived of oxygen and are responsible for the development of serious ailments, including cancer and heart disease.
Antioxidants convert the free radicals into harmless waste products that are eliminated from the body before any damage is done to the body. Thus, antioxidants act as scavengers that rid our body of free radicals that cause serious metabolic disorders by damaging the tissues and cells.
Plants are one of the primary sources of antioxidants.
Fruits, vegetables, nuts, legumes, cereals, and seeds are foods that are naturally rich in antioxidants.
The best way to ensure adequate intake of the antioxidants is to consume a variety of fruits and vegetables through a diet consisting of 5 to 8 servings of fruits and vegetables per day.
Fruits and vegetables can help guard against heart disease, cancers, and the effects of radiation, pollution, and aging.
Pomegranate, grape, orange, pineapple, plum, apple, and guava are some of the fruits that have the highest concentration of antioxidants.
In addition to being deliciously sweet, berries such as raspberries, blueberries, and strawberries are rich in antioxidants.
These berries are rich in proanthocyanidins - the antioxidants that can help prevent cancer and heart disease as well.
Broccoli, cabbage, carrots, spinach, lemon, ginger, peppers, parsley, kale, red beets, and tomato are vegetables rich in antioxidants.
Broccoli, a cruciferous vegetable, is one of the best antioxidants. It contains more vitamin C than an orange and has more calcium than a glass of milk.
In addition to minerals and vitamins, broccoli is filled with disease-fighting chemicals called phytonutrients.
Sulforaphane, a phytonutrient found in broccoli, has been shown to lower the risk of many types of cancers.
Tomato is the richest source of a powerful anticancer agent called lycopene.
Broad beans, pinto beans, soybeans are some of the best antioxidant foods.
Barley, millet, oats, corn are cereals rich in antioxidants.
Pecans, walnuts, hazelnuts, groundnut or peanut and, sunflower seeds contain a good amount of antioxidants.
Garlic, ginger, cloves, cinnamon, and oregano are antioxidant spices.
It also has been used as a natural antibiotic to kill off some strains of harmful bacteria.
Garlic is also useful for decreasing blood pressure and cholesterol, removing heavy metals from the body, preventing cancer, and acting as an antifungal and antiviral agent.
One clove of garlic contains vitamins A, B, and C, selenium, iodine, potassium, iron, calcium, zinc, and magnesium.
Green tea contains high concentrations of catechin polyphenols. It is also a powerful antioxidant and is very effective against cancer, heart disease, and high cholesterol.
Vitamin A includes carotenoids and retinol.
They are essential for healthy eyes and prevent macular degeneration or age-related blindness.
The antioxidant in vitamin A neutralizes free radicals and boosts your immunity.
Beta-carotene, which is sometimes called provitamin A, can be found in fruits and vegetables such as tomatoes, broccoli, guavas, carrots, pumpkins, apricots, and all green leafy vegetables.
All B vitamins are essential to a woman’s health.
They are essential for brain functioning, red blood cell formation, and DNA building. The important B vitamins are:
Vitamin C, also called ascorbic acid, serves as an antioxidant that facilitates wound healing.
It helps in the formation of collagen, which is essential for the wounds to heal.
It also helps in the production of new red blood cells, which deliver oxygen to your brain and to the other cells of your body.
Vitamin C is present in citrus fruits, grapefruits, strawberries, tomatoes, kiwi, oranges, and broccoli.
Also called cholecalciferol, this vitamin functions as a hormone and regulates bone homeostasis, together with calcium.
It is an important vitamin for women as it maintains strong and healthy bones.
A deficiency of this vitamin can cause you to have osteoporosis.
Exposure to sunlight helps your body produce vitamin D.
The dietary sources of vitamin D are eggs, fish, and vitamin-fortified products like milk.
Vitamin E or tocopherol acts as an antioxidant that aids in the production of red blood cells and the maintenance of the integrity of cellular membranes.
It also helps to slow age-related changes in the body.
Sources of this vitamin include nuts and nut products, wheat germ, cod liver oil, corn oil, and safflower oil.
In reality, eating healthy is never a cumbersome task. It all starts with a simple step of ringing in variety to your table.
Upload your DNA raw data to Xcode Life to get insights into 700+ health-related traits!
Diagnosed with Lactose Intolerance around a year back, instead of cutting out just the dairy products from my diet, I decided to go vegan altogether; well, mainly because I wanted to get on the “Vegan Lifestyle” bandwagon. Initially, I was uber excited about this cruelty-free lifestyle and a part of me was also secretly thrilled to finally live the life of the girls I’d admired on Instagram. So from one day to the next, I Instagrammed every meal of my day, shared recipes, and the love and support I got from the fellow vegans was overwhelming.
Fast forward to a couple of months later, it finally dawned on me that living a vegan life isn’t as glamorous as it is portrayed to be. I had to learn this lesson the hard way. Aside from having the “Instagram-perfect” life, nothing about this remotely contributed to a “pleasant experience”. Something about my body began to shift, and not in the direction I would’ve liked. The shift continued, till I woke up one day and decided that I couldn’t continue eating in a way that was not contributing to my health.
The first two-three months of following a vegan diet did shower me with a few solid perks which motivated me to stay true to the diet.
Hormone regulation controls the oil production by your sebaceous glands. Dairy and meat products, more often than not, come packed with a bunch of foreign hormones and it can send your own hormones totally out of whack. Eliminating these from your diet can thereby allow your body to regulate the hormones normally without any external interruptions.
Now, I am not gonna mislead you by saying that a vegan diet is a one-stop solution to treating acne. But for someone like me with acne-prone skin, this diet definitely did help me witness a marked reduction in the breakouts.
You may also be interested in: MC1R Gene: The Secret Key To A Healthier Looking Skin
Digestive issues have bothered me for the better part of my life, thanks to my undiagnosed lactose intolerance. A week into the vegan diet, I started witnessing lesser bloating and better digestion. I was also able to tame my inflammations well under control, which led to fewer IBD flare-ups.
My calorie intake varied between 1200-1500 a day, on the vegan diet. Women need to eat 2,000 calories each day to maintain weight. To lose weight, this number drops to around 1,500 calories a day. Though I wasn’t consciously trying to limit my calorie intake for weight loss, adopting this diet automatically meant the consumption of fewer calories. So, I ended up losing around 20 pounds over a span of 3 months.
Hand-picked article for you: Is Detox Water The Ultimate Weight Loss Secret?
I was happily sunbathing in the benefits, without realizing that my honeymoon period with the vegan diet was approaching an end. About 6 months into the diet, things started to take an unhealthy swing. Despite my body screaming for something different, I chose to listen instead to my morals screaming at me to keep eating a fully plant-based diet. But not before long, I started noticing physical indicators of this diet not working for me. And I couldn’t tune deaf to the screams any longer. One of the first signs I noticed, around 6 months into the diet, was massive hair fall. Bouts and bouts of hair falling everywhere; the shower, the bed, chairs I sit on, E-V-E-R-Y-W-H-E-R-E.
As superficial as it may sound, hair loss as a young woman is extremely terrifying. So, I immediately turned to my doctor, who advised a blood test. The results pointed to low levels of four main nutrients:
So he started me on a couple of supplements. These did help reduce the hair fall to an extent, but I still ended up losing a significant volume of my locks.
Find out your risk for Iron Deficiency here
On this diet, I kind of felt hungry throughout the day. And I also had increased cravings for junk foods. I did try my level best to not succumb to the cravings, but after a while I found myself googling “vegan-friendly snacks”. Next thing I know, I was filling my shopping cart with “vegan” chocolate sauce, “vegan” ice cream, “vegan” chocolate cookies. The pounds that I’d shed, were quick to re-latch to my body determined to never leave.
I personally love aerobic workouts and run on the treadmill for a good 60-90 minutes before exhaustion begins to set in. Even then, a 2-3 minute rest period would put me back right on track for my next workout. A couple of weeks into the diet, I could see myself underperforming in the gym with exhaustion setting in 20 minutes into my work out, and not the kind of exhaustion that a 2 minute rest period would resolve. The exhaustion was accompanied by nausea and dizziness that did not allow me to resume my workout after that.
Get personalized and actionable fitness recommendations
I often found myself down with flu or some infection while on this diet. A blood test that I decided to take up indicated low counts of my WBCs. My doctor later explained to me how low protein intake could deplete the WBCs leaving the immune system at an inability to fight off infections. When I read up further on this, I also came across a study that linked a deficiency in protein to HIV infections, as the body is less prepared to fight off the virus, leaving you more likely to become infected. And oh boy, did that put me on the edge of my seat. Scary, right?
So basically yeah, all this ended up in me bidding adieu to veganism. But as I’d mentioned in the very beginning, this is just my experience with the vegan diet. It works for some and for others, it simply doesn’t. In all honesty, nothing you read will ever prepare you for the commitment you need to make this work and that is why there are a lot more former-vegans than vegans itself.
Of course, I did enjoy a few perks of being on this diet. So instead of turning a blind eye to this whole thing, you can instead borrow some aspects of vegan and vegetarian eating, such as eating plenty of fruits, vegetables, and whole grains and incorporate them into your diet, to get some health benefits.
And always keep in mind, before you start any diet, check for your nutritional deficiencies and consult a doctor to take appropriate supplements.
Upload the file to Xcode Life to get insights into 700+health-related traits!.
The Gene Nutrition Report covers over 33 categories. It helps identify your genetic risk for 9 vitamin deficiencies. The report also gives insights into the requirements of many minerals like calcium, magnesium, iron, copper, etc. It contains information about your tendency to gain and lose weight upon consumption of the essential nutrients, including carbs, proteins, and fats. Each category covered also comes with some food recommendations which can help highly optimize your diet.
Needless to say, calcium is one of the most abundant minerals in the body. It does a whole lot more than just strengthening our bones and teeth. Hence the deficiency of calcium can affect many of our body functions.
Calcium is necessary for many important processes like:
Though 99% of the calcium in our body is stored in the bones, other tissues like muscles and blood also contain calcium.
The body continuously regulates the calcium present in the blood as well as the cells by moving it in and out of the bones as and when there is calcium deficiency.
When the intake of calcium is less or when there is a calcium deficiency, the body maintains its levels in the blood and cells by mobilizing them from the bones, thereby weakening them.
Calcium is obtained from the foods we eat.
Many foods are naturally rich in calcium, and it is important to include such foods during each meal.
Some of the good sources of calcium are:
The amount of calcium required by an individual depends upon their age, gender, and other factors like underlying health conditions and overall health.
The normally followed dietary recommendations for calcium are:
CASR or Calcium-Sensing Receptor is an extracellular G-protein that plays a vital role in calcium homeostasis. The gene that encodes this protein, located on chromosome 3, is usually expressed at very high levels in the parathyroid glands, thyroid, intestine, and kidneys.
The CASR protein forms a stable homodimeric receptor. The receptors signal into the cells when calcium ions bind to them. This causes a downregulation of gene expression that influences calcium homeostasis in the parathyroid areas. Simultaneously, there's a rise in the levels of calcium in the kidney, and the excretion of sodium chloride (salt) is lessened.
Also, the binding of calcium to the CASR gene occurs within the normal physiological limits of the calcium ions. This leads to a steep dose-response curve and results in tight control of calcium levels in the blood.
Variations in this gene have been extensively studied. One variation, a G to T transition, alters the receptor efficacy. This can influence parathyroid hormone secretion, increase calcium clearance, and finally affect calcium homeostasis.
The CYP24A1 gene is located on chromosome 20 and belongs to the cytochrome P450 superfamily of enzymes. Particularly, the gene provides the instructions required for making the 24-hydroxylase enzyme.
This enzyme is responsible for controlling the amount of active vitamin D available in the body. Vitamin D is absolutely essential for the proper absorption of calcium from the intestines and is also necessary for various processes required for bone and tooth formation. Variations in this gene that affect vitamin D consequently causes inefficient calcium absorption.
Several other mutations are also found associated with this gene. One of which is known to cause idiopathic infantile hypercalcemia.
GATA3 or GATA binding protein 3 is a gene that is located on chromosome 10 and belongs to the GATA family of transcription factors.
Any defects in this gene result in hypoparathyroidism along with sensorineural deafness and renal dysplasia.
Hypothyroidism causes a reduction in the calcium levels in the blood, i.e., hypocalcemia.
The condition when the calcium levels in the blood are low is called hypocalcemia. It is more common in women, and also more so as people age.
Other causes that can lead to hypocalcemia include:
You might also be interested in: Are You Meeting Your Vitamin D Needs? Let Us Ask Your VDR Gene!
Early-stage hypocalcemia does not show any symptoms, which only appear when the disease progresses.
Some symptoms of hypocalcemia include:
It is advisable not to self-treat calcium deficiency by taking OTC calcium supplements as it can negatively impact one's health by interacting with any other medications one may be taking.
Based on the calcium levels, your physician will provide you with the right calcium supplement and ask you to increase your dietary intake.
Commonly advised calcium supplements are:
Including calcium-rich foods in each of the meals also tremendously helps to treat the deficiency.
The following groups of people may be at a risk for calcium deficiency and can consider taking prescribed supplements:
Calcium supplements are primarily of two types: Calcium carbonate-based and calcium citrate-based. Each type of calcium supplement, contains a different calcium salt and different amounts of elemental calcium.
The supplements that are calcium carbonate-based are cheaper and therefore, more popular. They contain 40% elemental calcium. The citrate-based supplements contain about 21% of elemental calcium. Other calcium supplements contain salts like calcium lactate (containing 13% elemental calcium) and calcium gluconate (9% elemental calcium).
Combining calcium supplements with vitamin D intake can help increase the absorption of calcium. Magnesium is also a good substitute for vitamin D.
Calcium can cause calcification of blood vessels and thus, the usage of calcium supplements raise some serious cardiac concerns. However, no study has shown a solid proof of calcium supplements posing a threat to the heart health.
On the other hand, there has also been no conclusive proof to show that calcium supplements indeed help in preventing diseases like osteoporosis.
According to a 2015 study, calcium supplements increase the risk of kidney stone recurrence, especially in people who are prone to it.
There is a split in the medical world over whether calcium supplements cause heart disease or not.
While some say these calcium supplements do not precipitate heart disease, others say that the calcium from the supplements can harden or calcify the existing plaque in the blood vessels.
However, research suggests the following about the relationship between calcium supplements and heart disease:
When the calcium level in the blood is over 10.3 mg/L, the condition is called hypercalcemia. Excessive calcium in your blood can be harmful to your bones, kidneys, and also affect the way the other organs in your bodywork.
Hypercalcemia is usually the effect of overactive parathyroid glands that result in an increase in the blood calcium levels. Other causes of hypercalcemia include:
The symptoms of hypercalcemia differ with each organ.
In individuals with mild hypercalcemia, the calcium levels usually return to normal over time and do not need any treatment.
The physician may continue to monitor the calcium levels and the health of the kidneys while the calcium levels return to normal. However, when calcium levels do not return to normalcy on their own, the doctor will recommend further testing to determine the underlying cause of high calcium levels.
Possible treatments to reduce calcium levels include IV fluids and medications like calcitonin and bisphosphonates. If hypercalcemia is due to excessive vitamin D, hyperactive parathyroid glands or any other underlying condition, the doctor will focus on removing or treating this cause.
One of the basic things to do to keep your calcium levels in check is maintaining a healthy and balanced lifestyle.
One of the best ways to ensure healthy and optimum calcium levels is by sufficient dietary intake of the mineral. Some foods that are exceptionally high in calcium are:
https://ghr.nlm.nih.gov/gene/CYP24A1#conditions
https://ghr.nlm.nih.gov/gene/GATA3#synonyms
Upload your DNA raw data to Xcode Life. Our Gene Nutrition Report analyzes your requirements for vitamin A, vitamin B12, vitamin B6, and 30+ such traits.
Updated 08 May 2020
