Reports
Health
Wellness
Breast cancer is one of the most common types of cancer affecting American women. On average, 13% of American women will develop this invasive condition.
Many genetic and environmental factors can increase or decrease a person’s risk of developing breast cancer.
One such factor is the amount of fat you consume.
Dietary fat is a macronutrient needed in the right amounts to keep the body healthy and nourished.
The fat you consume is usually stored as a reserve in the adipose tissue and used as an energy source when you consume fewer calories than what the body needs.
Fat also helps absorb fat-soluble vitamins like vitamin A, D, E, and K.
Fats play a role in protecting your internal organs, keeping you warm, and controlling the action of different hormones.
High levels of dietary fat may increase the sex hormones in a woman’s body (estrogen and progesterone). Some researchers assume that this may be why fats increase the risk of breast cancer, especially hormone-receptor-positive breast cancers.
High dietary fat intake also increases the risk of obesity. Obesity, in turn, increases postmenopausal ER-positive breast cancer risk by increasing estrogen production in the body.
A 2003 study assessed the risk of breast cancer in 90,655 premenopausal women between the ages of 26 and 46. This 8-year study identified 714 cases of breast cancer during the follow-up.
According to the study, women who had consumed high animal dietary fats had a slightly increased risk for breast cancer. The study identified that red meat, animal fat, and dairy products specifically increased cancer risk.
Does The Type of Fat Matter?
There are four major types of dietary fatty acids.
Saturated and trans fat are considered unhealthy fats as they increase blood cholesterol levels and lead to heart conditions.
Unsaturated fats are healthy as they bring down cholesterol levels and also boost heart health.
When it comes to breast cancer risk, the type of fat you consume definitely matters. Many studies relate saturated fats and trans fats to an increased risk for breast cancer. Conversely, some unsaturated fats seem to be protective against breast cancer.
A 2003 meta analysis studies the risk of breast cancer in people who consumed excess dietary fats.
According to the meta-analysis, short-term and long-term studies found that people who consumed excessive saturated fats and meat had a 13% higher risk of breast cancer.
Another combined analysis study that included data from 12 case-controlled studies found a positive relationship between saturated fat intake and breast cancer.
This study also reports that with changes in the diet, up to 24% of postmenopausal women and 16% of premenopausal women in North America decreased their risk of developing breast cancer.
Industrial Trans Fatty Acids (ITFAs) are trans fats produced in industries and added to various dairy products, snacks, and pastries. Ruminant Trans Fatty Acids (RTFAs) are made in the bodies of cows, goats, sheep, and other animals as a result of bacterial action. RTFAs are present in most animal fats, and consuming these fats increase RTFA levels in the body.
The European Prospective Investigation into Cancer and Nutrition (EPIC) found a positive relationship between ITFA and RTFA consumption and the risk of breast cancer in 318,607 women.
A 2005 study analyzed the effects of unsaturated fatty acids on breast cancer risk. The study reported that omega-3 fatty acids, a type of polyunsaturated fatty acid, brought down the risk of breast cancer.
In contrast, omega-6 fatty acids, a different kind of polyunsaturated fatty acid, increased the risk of breast cancer.
A 2015 article observed the interaction of omega-3 fatty acids and omega-6 fatty acids in the development of breast cancer in 1463 breast cancer patients and 1500 controls. The study suggests that American women can reduce their risk of breast cancer by increasing their omega-3 fatty acid intake (omega-3 has anti-inflammatory properties) and decreasing the consumption of omega-6 fatty acids (Omega-6 induces inflammation).
When it comes to MUFAs, the type of food plays a role in increasing or decreasing cancer risk.
A 1993 meta-analysis study reported that MUFAs also increase a woman’s risk of developing breast cancer.
Another study reported that oleic acid and palmitic acid, types of monounsaturated fatty acids, increased the risk of breast cancer in women.
Olive oil, which is rich in MUFA, seems to protect against cancers, though. People who chose olive oil over other lipids like butter had high levels of protection against all cancers, including breast cancer.
The DOCK1 gene (Dedicator of cytokinesis gene) helps create the DOCK180 protein that plays a role in signaling between cells.
rs113847670 is a single nucleotide polymorphism or SNP in the DOCK1 gene. It is associated with breast cancer risk. The T allele of this SNP results in 5 times higher risk of developing breast cancer on excess intake of saturated fats.
| Allele | Implications |
| T | 5-times higher risk of developing breast cancer on excess intake of saturated fats |
| C | Normal risk of breast cancer on excess intake of saturated fats |
Obesity is one of the factors that can contribute to increased breast cancer risk. Excess intake of fats can lead to weight gain and obesity too. As a result, the combination of obesity and excess fat intake can aggravate breast cancer risk.
This is true, especially in post-menopausal women. Such women can bring down their risk of breast cancer by limiting saturated and trans-fat intake.
Other than cutting back on fats, the following dietary changes can help lower breast cancer risk:
Genetic testing will tell how harmful fat consumption is for your body. If you are at higher risk of developing breast cancer because of fat intake, talk to a nutritionist to control the risk.
When opting for a healthy lifestyle, much of the difficulty we face is attributed to our diet. Why aren't we craving healthy foods? Why do some of us feel a surge of revulsion every time we see kale before us? It appears our food preferences run deeper, well into our genetic code.
Taste preference is a complex interplay of physiological, psychological, genetic and social factors of an individual. Among these, genes particularly play a significant role in influencing an individual’s taste and food preferences. By understanding the genes that play a role, it will help us align our diet based on our genes, and perhaps, this will help us eat healthier!
Of the 5 different senses we have, taste is the most personal of it all. It's uniquely ours, and is the determinant of what we choose to eat. Just as there are differences among humans in various physical traits due to genetics, there are myriad differences in taste preferences, sometimes major and often minor. Efforts have been underway since the early days to determine the origin of our taste preferences, and we now know they're genetically encoded.
Taste preferences are known to influence energy intake and there are many genes that are important in determining taste preferences, with the gene TAS2R38 being a significant one.
The TAS2R38 gene, short for Taste 2 Receptor Member 38, is located on chromosome 7 and is known as the 'bitter' gene. This gene encodes a receptor that may play a role in the perception of bitter taste. They also play a role in sensing the chemical composition of the gastrointestinal tract. Research shows that TAS2R38 gene influences 70% of the preference for bitter foods.
Studies on TAS2R38 began when some people found phenylthiocarbamide (PTC), a synthetic compound, bitter while other others had no taste for PTC. Since then, although many different forms of this gene have been identified, there are predominantly two forms - taster and non-taster. The taste was initially thought of to be an effect of natural selection, as identifying bitter taste would help in staving off toxic substances in the food. However, the non-taster variant is also quite popular in the general population and the notion of natural selection of taster variant was dropped. Recent studies reveal that demographic pressures largely influence this gene's expression
There are certain variants of TAS2R38 gene with an association to greater BMI. The three variants of the gene can result into classification of non-tasters, tasters and super -tasters. The non- tasters have high threshold and low sensitivity while tasters have low threshold and high sensitivity. The third category is the super tasters who have an increased sensitivity. The taste perception of these three variants differs considerably, for example non-tasters perceive scotch as less bitter and more sweet than super tasters.
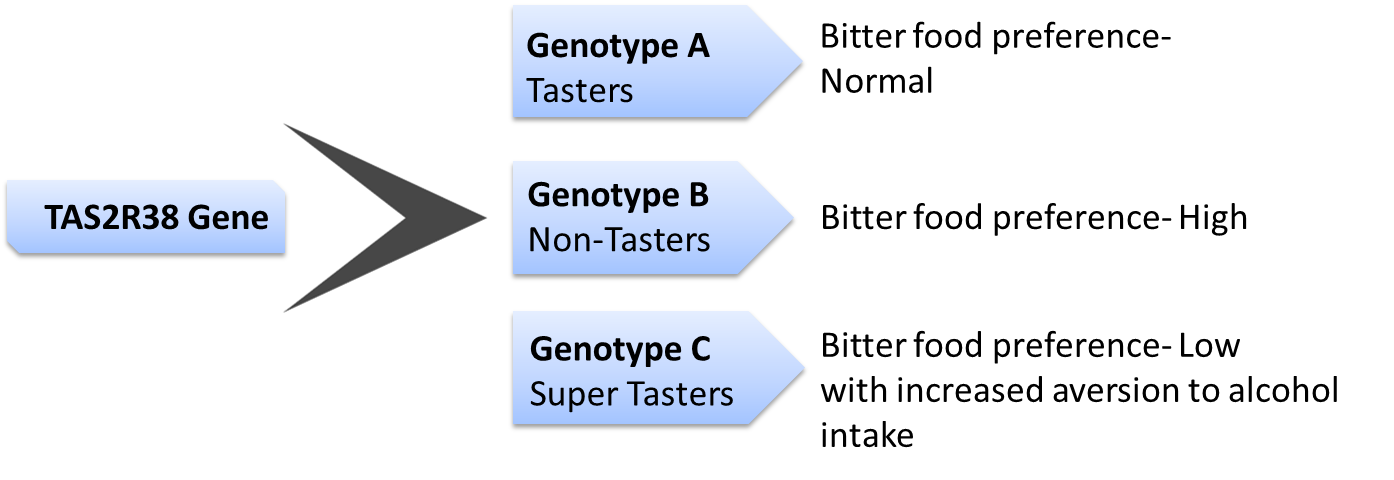
People with the non-taster version of the gene should modulate their energy intake to prevent excess intake of alcohol, or other high calorie bitter foods which can potentially increase their risk of obesity and other associated conditions.
Several genes influence our preference for sweet tastes. These include TAS1R1, TAS1R2. TAS1R3. The genes work interdependently. For example, the protein produced by TAS1R3 binds to the protein TAS1R1 to form a pleasant savoury taste, umami response or it could bind with TAS1R2 to form a sweet taste response.
The variants of TAS1R1 play an important role in food preferences. Apart from food preference, TAS1R2 is present in various parts of the body and could play a role in sugar metabolism, contributing to inter-individual difference in energy intake.
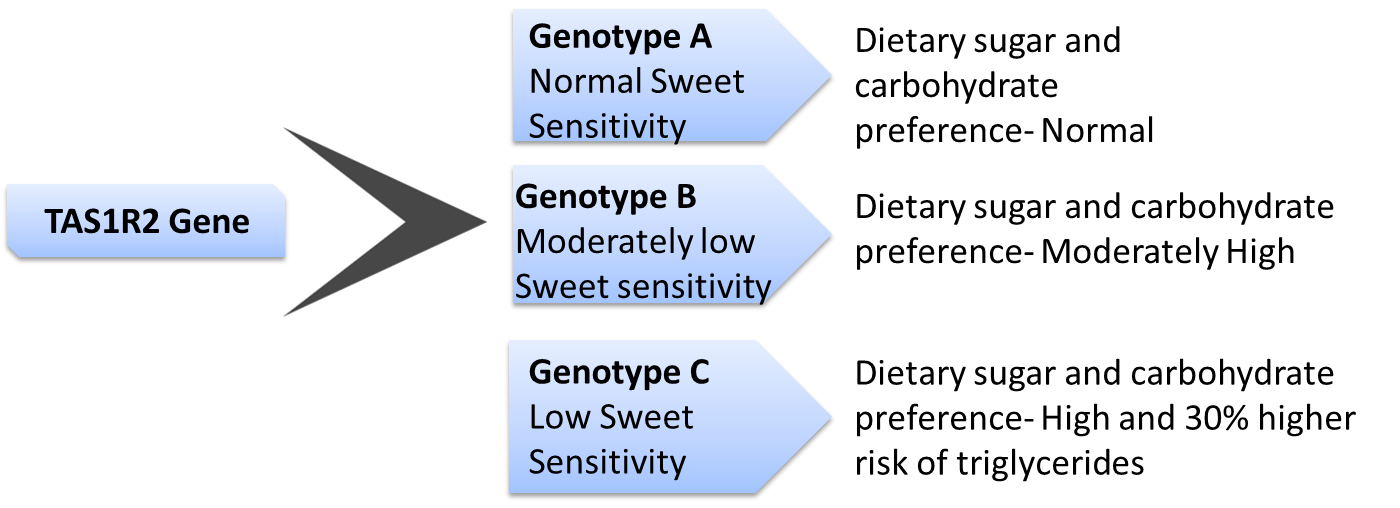
Individuals with the ‘high risk’ genotype can modulate the effect of the risk variant by controlling the amount of carbohydrate consumed.
An important food preference that can directly affect the risk for obesity is fat taste preference. Fat from dietary sources is not only essential for energy storage but is also vital for temperature regulation. An important gene that regulates our perception of taste of fatty food is the CD36. Located on chromosome 7, this gene influences the amount of fat consumed.
Having certain variants of CD36 gene can increase or decrease the levels of CD36 protein produced. For example, some variants produce low levels of CD36 are, therefore, less sensitive to fat with higher threshold for increased fat intake. On the other hand, individuals with high levels are more sensitive to fat in their diet, and hence consume less fat.
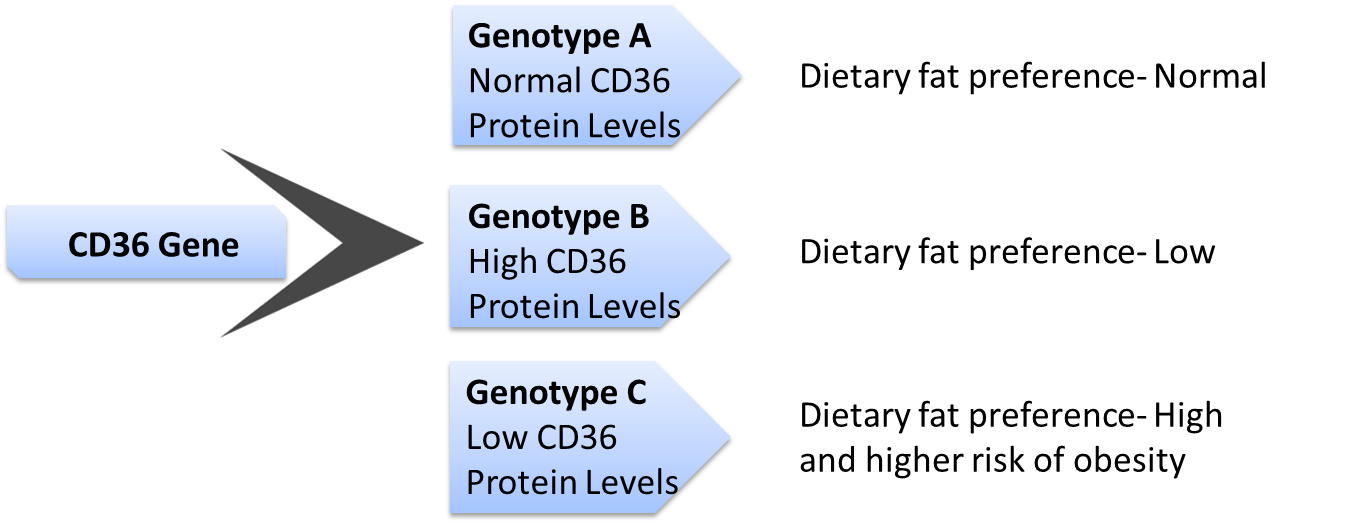
Individuals with a high preference for food rich in fat should modulate their risk for obesity by controlling fat content in their diet. Studies have also shown that such individuals could lower risk for cardiovascular disease and obesity by following a mediterranean diet.
The genetic variants that control our taste preference also have an association with obesity and other metabolic conditions. Metabolic syndrome is a combination of health issues that can increase our risk for certain serious health conditions like a cardiovascular disease or diabetes. Therefore, it has become all the more important to know the gene variants responsible for our food preference.
Taste is an individual preference, influenced by the genes that we carry, and dictating energy intake. An average human has over 9,000 taste buds and it is therefore no surprise that we love to eat! However, understanding the genes we carry will aid in making intelligent food choices for better health.
Want to know your genetics of taste preferences? Find out by uploading your DNA raw data to Xcode Life!
