Reports
Health
Wellness
Diet is as important to mental health as it is to physical health. Previous studies have reported that the "traditional" dietary pattern, loaded with vegetable oil, meat, salt, and organ meat, is associated with increased odds of anxiety and depression in women. A recent study by researchers at the Ruhr-University Bochum and University of Duisburg, Germany, has reported higher depression scores among vegetarians than non-vegetarians.
Depression is a common yet serious mental condition that negatively impacts how you feel, the way you think and act. Depression occurs as a result of a combination of social, psychological, and biological factors.
Some of the common symptoms of depression are :
Depression susceptibility is related to diet both directly and indirectly. Unhealthy eating patterns can cause mood swings. When you stick to a healthy diet, you are setting yourself up for fewer mood fluctuations.
In particular, sugar is considered a major culprit. When consumed in higher quantities, it causes a temporary spike in 'feel-good' hormones like dopamine, which is not good for your health. In addition, the fleeting sugar rush followed by a crash is terrible for your mood.
A German research team conducted a meta-analysis on depression and vegetarian diet.
Meta-analysis refers to a procedure where the information collected from different experiments (with the same objective) is put together and studied. This combines the results of multiple studies to form a conclusion.
The analysis included data from 49,889 participants, of which 8,057 were vegetarians, and 41,832 were non-vegetarians. The large sample size makes this a robust study.
The researchers observed a higher depression score among vegetarians when compared to the non-vegetarians. But there was no causal relationship observed between them. That is, there was no proof that a vegetarian diet directly causes depressive moods. Depression didn't seem to increase a person's chance of adopting a vegetarian diet either.
This study, however, showed that it might be more likely that people switch to a vegetarian diet after developing mental health issues. The researchers cite three possible reasons for this:
Breast cancer is one of the most common types of cancer affecting American women. On average, 13% of American women will develop this invasive condition.
Many genetic and environmental factors can increase or decrease a person’s risk of developing breast cancer.
One such factor is the amount of fat you consume.
Dietary fat is a macronutrient needed in the right amounts to keep the body healthy and nourished.
The fat you consume is usually stored as a reserve in the adipose tissue and used as an energy source when you consume fewer calories than what the body needs.
Fat also helps absorb fat-soluble vitamins like vitamin A, D, E, and K.
Fats play a role in protecting your internal organs, keeping you warm, and controlling the action of different hormones.
High levels of dietary fat may increase the sex hormones in a woman’s body (estrogen and progesterone). Some researchers assume that this may be why fats increase the risk of breast cancer, especially hormone-receptor-positive breast cancers.
High dietary fat intake also increases the risk of obesity. Obesity, in turn, increases postmenopausal ER-positive breast cancer risk by increasing estrogen production in the body.
A 2003 study assessed the risk of breast cancer in 90,655 premenopausal women between the ages of 26 and 46. This 8-year study identified 714 cases of breast cancer during the follow-up.
According to the study, women who had consumed high animal dietary fats had a slightly increased risk for breast cancer. The study identified that red meat, animal fat, and dairy products specifically increased cancer risk.
Does The Type of Fat Matter?
There are four major types of dietary fatty acids.
Saturated and trans fat are considered unhealthy fats as they increase blood cholesterol levels and lead to heart conditions.
Unsaturated fats are healthy as they bring down cholesterol levels and also boost heart health.
When it comes to breast cancer risk, the type of fat you consume definitely matters. Many studies relate saturated fats and trans fats to an increased risk for breast cancer. Conversely, some unsaturated fats seem to be protective against breast cancer.
A 2003 meta analysis studies the risk of breast cancer in people who consumed excess dietary fats.
According to the meta-analysis, short-term and long-term studies found that people who consumed excessive saturated fats and meat had a 13% higher risk of breast cancer.
Another combined analysis study that included data from 12 case-controlled studies found a positive relationship between saturated fat intake and breast cancer.
This study also reports that with changes in the diet, up to 24% of postmenopausal women and 16% of premenopausal women in North America decreased their risk of developing breast cancer.
Industrial Trans Fatty Acids (ITFAs) are trans fats produced in industries and added to various dairy products, snacks, and pastries. Ruminant Trans Fatty Acids (RTFAs) are made in the bodies of cows, goats, sheep, and other animals as a result of bacterial action. RTFAs are present in most animal fats, and consuming these fats increase RTFA levels in the body.
The European Prospective Investigation into Cancer and Nutrition (EPIC) found a positive relationship between ITFA and RTFA consumption and the risk of breast cancer in 318,607 women.
A 2005 study analyzed the effects of unsaturated fatty acids on breast cancer risk. The study reported that omega-3 fatty acids, a type of polyunsaturated fatty acid, brought down the risk of breast cancer.
In contrast, omega-6 fatty acids, a different kind of polyunsaturated fatty acid, increased the risk of breast cancer.
A 2015 article observed the interaction of omega-3 fatty acids and omega-6 fatty acids in the development of breast cancer in 1463 breast cancer patients and 1500 controls. The study suggests that American women can reduce their risk of breast cancer by increasing their omega-3 fatty acid intake (omega-3 has anti-inflammatory properties) and decreasing the consumption of omega-6 fatty acids (Omega-6 induces inflammation).
When it comes to MUFAs, the type of food plays a role in increasing or decreasing cancer risk.
A 1993 meta-analysis study reported that MUFAs also increase a woman’s risk of developing breast cancer.
Another study reported that oleic acid and palmitic acid, types of monounsaturated fatty acids, increased the risk of breast cancer in women.
Olive oil, which is rich in MUFA, seems to protect against cancers, though. People who chose olive oil over other lipids like butter had high levels of protection against all cancers, including breast cancer.
The DOCK1 gene (Dedicator of cytokinesis gene) helps create the DOCK180 protein that plays a role in signaling between cells.
rs113847670 is a single nucleotide polymorphism or SNP in the DOCK1 gene. It is associated with breast cancer risk. The T allele of this SNP results in 5 times higher risk of developing breast cancer on excess intake of saturated fats.
| Allele | Implications |
| T | 5-times higher risk of developing breast cancer on excess intake of saturated fats |
| C | Normal risk of breast cancer on excess intake of saturated fats |
Obesity is one of the factors that can contribute to increased breast cancer risk. Excess intake of fats can lead to weight gain and obesity too. As a result, the combination of obesity and excess fat intake can aggravate breast cancer risk.
This is true, especially in post-menopausal women. Such women can bring down their risk of breast cancer by limiting saturated and trans-fat intake.
Other than cutting back on fats, the following dietary changes can help lower breast cancer risk:
Genetic testing will tell how harmful fat consumption is for your body. If you are at higher risk of developing breast cancer because of fat intake, talk to a nutritionist to control the risk.
The Fatty Acid Desaturase (FADS1) gene is associated with the synthesis of FADS1 protein, an enzyme secreted in the liver and shown to be associated with the conversion of shorter chain fatty acids to longer length active forms. The FADS1 protein is found to be associated with the conversion of omega 3 and omega 6 from plant based fats to functional and longer forms like EPA, DHA and arachidonic acid (AA). Animal meat, fish and eggs are already rich in EPA, DHA and arachidonic acid, which reduces the need for the FADS1 protein. People with the C variant of the gene are found to be associated with reduced activity of the protein.
Individuals who do not produce sufficient amount of fatty acids need to consume more animal foods to meet requirements, while individuals who can convert plant-based oils to EPA, DHA and arachidonic acid would benefit from consuming a diet that is rich in vegetable oils and lower in omega-6-rich animal meats.
When excess of omega-6-rich foods is consumed, it is found to be associated with inflammation which is found to increase the risk for diabetes and heart disease. Individuals who can synthesize long chain fatty acids from plant sources should, therefore, select sea food to meet PUFA requirements.
The FADS1 single nucleotide polymorphism that we include is found to have a significant association with the fatty acid composition in our blood. The ancestral allele C (rs174547) was predominant among the hunter gatherers and, with the start of farming, the allele T became the predominant allele.
| CHIP Version | FADS1 SNPs |
| 23andMe (Use your 23andme raw data to know your FADS1 Variant) | |
| v1 23andme | Present |
| v2 23andme | Present |
| v3 23andme | Present |
| v4 23andme | Present |
| V5 23andme (current chip) | Present |
| AncestryDNA (Use your ancestry DNA raw data to know your FADS1 Variant) | |
| v1 ancestry DNA | Present |
| V2 ancestry DNA (current chip) | Present |
| Family Tree DNA (Use your FTDNA raw data to know your FADS1 Variant) | |
| OmniExpress microarray chip | Present |
In a study conducted on 3521 Chinese participants and 8962 participants of European ancestry, individuals with the C variant of the gene were found to have lower levels of the long forms of fatty acids like AA.
In another study conducted on nearly 1200 Chinese men, Individuals with the T variant of the gene were more responsive to the cholesterol lowering effect of dietary eicosapentaenoic acid (EPA), with reduction in coronary artery disease risk among individuals with high intake of long chain polyunsaturated fatty acids. In a review study conducted on Japanese men, vegans with the C variant of the gene were found to have lower plasma concentrations of EPA, DHA and AA than individuals who were omnivores. Vegetarians with the C variant of the gene are shown to benefit from consuming omega 3 supplements or omega 3 rich foods like chia seed, flax seeds and canola oil.
| Genotype rs174547 | Phenotype | Recommendation |
| TT | [Advantage] More likely to have increased activity of the fatty acid saturase enzyme [Advantage] More likely to derive long chain fatty acids from a vegetarian diet | People with this variant of the gene would benefit from a vegetarian diet. In case of non-vegetarians, a diet that includes seafood instead of red meat is recommended. Fish oil can be consumed as supplements or by eating fish. Fish that are especially rich in omega 3 fatty acids include tuna, herring mackerel, cod liver, seal blubber and whale blubber |
| CC | [Limitation]More likely to have decreased activity of the fatty acid saturase enzyme [Advantage] More likely to benefit from a diet rich in animal fats | People with this variant would benefit from a diet rich in animal fats, especially fish. In case of vegetarians, consuming twice the amount of canola oil when compared to people with the T variant would help increase the level of EPA. Omega 3 supplements may be consumed to compensate for the reduction in EPA due to lowered enzyme activity. Omega 3 foods that are rich vegetarian sources include chia seeds, flax seed oil and canola oil |
“Nutrigenetics, fitness genetics, health genetics are all nascent but rapidly growing areas within human genetics. The information provided herein is based on preliminary scientific studies and it is to be read and understood in that context.”
[hr height="30" style="default" line="default" themecolor="1"]Are fats good or bad? Which types of fats are good and which types are bad? And how much fat is bad and how much is good? Is fat bad for everyone or only for some or for some more so than others? These are among the many confusing questions that we encounter everyday. And one can find a variety of confusing information on the internet, from diet plans which recommend overloading on fats to fat avoidance.
For decades, nutritionists and doctors have preached that a low-fat diet is the key to maintaining optimal weight and preventing health problems. But in recent times, research has shown that a diet rich in healthy fats can be better for people, particularly if those fats are used to offset the consumption of foods containing high levels of salt, sugar and refined carbs. Recent U.S dietary guidelines (2015) no longer focus on the restriction of fat in the diet, instead emphasizing the quality of fat
[hr height="30" style="default" line="default" themecolor="1"]
[one_second]One of the key features that distinguishes humans from other primates is the larger brain size, and a relatively large portion of the our daily energy intake is consumed in the brain. This could have necessitated humans to consume foods with high energy density such as fats, especially long chain polyunsaturated fatty acids, in order to meet the high energy demands of the larger brains. The same could be attributed to our enhanced ability to prefer, detect, digest and metabolise high fat foods, and larger amounts of animal foods compared to other primates. Evidence indicates that the human evolution took place on an omega 3 rich diet found in East- African land-water ecosystems which made it easy to get iodine, vitamin A and omega 3 rich foods both from plants and fish necessary for brain functions. When humans migrated out of Africa, new evolutionary adaptations developed to enable survival in various environments with diverse food sources.
The dietary fats have undergone tremendous changes in terms of quantity and quality over the past 10,000 years. Some of the notable changes in the modern day diet in terms of dietary fat quality are the increased intake of saturated fatty acids, linoleic acid (LA), [/one_second]

[one_second]derived from omega 6 fatty acids and industrially produced trans fatty acids and reduced intakes of omega 3 fatty acids, dominance of more arachidonic acid, derived from LA in the diet. These changes are thought to have a broad impact on one’s health including chronic low grade inflammation leading to metabolic syndrome and its sequelae .[/one_second]
[hr height="30" style="default" line="default" themecolor="1"]
Long chain polyunsaturated fatty acids (LCPUFAs), arachidonic acid (AA), eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) provides structure for cells, act as messengers between and within cells, and play a major role in lipid and sugar balance in the body. Our body converts all the shorter length polyunsaturated fatty acids (SCPUFAs) to LCPUFAs by using FADS (fatty acid desaturase) enzyme, produced by the FADS genes such as FADS1 and FADS2.
Plant based fats such as those from foods like vegetable oils, seeds and nuts, are SCPUFAs, the shorter length fatty acids such as alpha linolenic acid (omega 3) and linolenic acid ( omega 6) and need to be converted to LCPUFAs such as EPA, DHA and AA respectively in order to be utilized by our body, whereas animal based fats such as fish, eggs or steak already contains longer length LCPUFAs and our body can readily utilise them without the need for conversion.There are different types of FADS1 gene and the type you carry determines how well the SCPUFAs are converted to LCPUFAs. People carrying the “C” type of this gene have reduced conversion ability, and such people need to get their PUFA from animal sources especially fish or from supplements. Whereas people carrying the “T” type of this gene have efficient conversion ability and they need not rely on animal sources of PUFA to meet their needs.
A recent study done at the Cornell University compared 234 individuals of a primarily vegetarian Indian population and 311 individuals of traditional meat eating American population. Using 1000 genomes project, the study provided evidence that people with long ancestry of plant based diet have developed a mutation in the FADS2 gene, that has helped them convert SCPUFAs to LCPUFAs, hence fulfill their Omega-3 requirements from plant based sources. The study also points out people with FADS2 “vegetarian-gene” type are at higher risk of cardiac disease and cancer when they switch to a non-vegetarian diet.
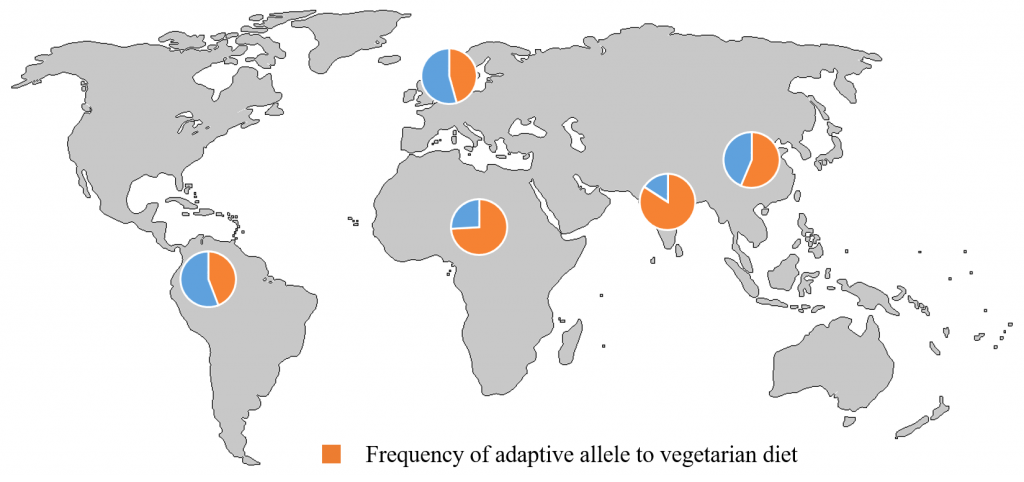
Credit: Kaixiong Ye, Cornell University/Map from www.outline-world-map.com The graph shows the global frequency pattern of an allele adaptive to vegetarian diets. The allele has the highest frequency in Indians, who have traditionally relied heavily on plant-based diets.
Thus, prescribing personalised diets based on the type of FADS genes – insertion type or the deletion type can be an important consideration for precision nutrition and medicine.
Want to know if you have the “the vegetarian gene” Xcode’s nutrigenetics test can tell you what versions of the FADS1 gene you have in your DNA. You can also learn about how your genes may influence other traits, including your risk for certain diseases. You can write to us at info@xcode.in
