Reports
Health
Wellness
Ever wondered how some people run multi-million dollar companies along with a gazillion other philanthropic work? Read on to understand more about entrepreneurship potential and the debate about its source of origin.
From selling cupcakes to running a multi-million dollar biggie, entrepreneurs form a diverse spectrum.
Any business idea, transformed into a business model to serve customers/clients fall under entrepreneurship.
But most of them, who run big or small successful businesses have some highly similar qualities.
It takes more than just an idea to be a successful entrepreneur.
The first "light bulb" moment is only a start to a snowball of those to follow. Initially, setting up an idea means having to act as five different roles in one.
Granted we have a lot of resources online, but to gather the motivation and humility to be able to understand and learn new things and then adapt that into your idea of a business model, takes quite some time.
So, first and foremost, patience is key.
And most definitely, you would have to disable ‘autoplay’ on youtube, too bad Netflix doesn't let you do that!
Understanding a market gap and tapping into that potential is extremely important with new ideas.
Your cupcakes might taste out of the world delicious, but what is the customers’ incentive to buy them, if they can find great cupcakes (tried and tested) from Costco?
What if you add a factor of customization, say you provide the customers icing essentials to make it their own?
That might make it interesting.
Understanding what the customers need and delivering, is one of the most crucial components of entrepreneurship.
When American computer scientist, Paul Graham was asked what are the most important things to remember to become a successful entrepreneur, he said, surrounding yourself with good, efficient people, finding the best market-product fit and spending as little money as possible.
These frame a 3-step activation for your success account. If either of them fails to happen, it could be significantly hard to create a successful empire.
A successful entrepreneur in one of his books talks about how running a startup is like juggling.
It creates an illusion that you’re balancing three balls mid-air but in reality, a juggler focuses on one ball to balance the rest.
This is how entrepreneurs deal with multitasking.
By prioritizing the right task at the right time. It is crucial to identify the most important problem and solve that first.
“Most of us spend too much time on what is urgent and not enough time on what is important.”
Stephen R. Covey
It’s all about smart working
Hard Work is not the only key to success. Many entrepreneurs have seen success in hiring people who do smart work.
"Hire a lazy person to do a difficult job they will find an easy way to do it"
Bill Gates
Entrepreneurs have to be constantly driven to work towards success.
All successful entrepreneurs have their dull days and depressing mornings.
They too get distracted with the sweet smell of freshly sprinkled earth or a fresh batch of cookies.
It’s about how they bring their attention back to work, which is admirable.
A famous tech expert, Aytekin Tank says finding this grit, to keep up with a goal for a lifetime comes from endless motivation and learning to overcome resistance.
Coming up with routines that get our body and mind prepped to do a task could make a significant difference.
Love is not the only kinda north star we need.
Having a life vision and mission for a company helps with clear growth and better focus towards the end goal.
In this ever-changing world, be it Twitter or LinkedIn there is a 200-300 character limit to say what you have in mind.
It’s highly crucial to stay focused and walk towards your north star.
It’s common to see entrepreneurs sound profound and knowledgeable.
But the successful ones are almost always curious to understand more.
This constant need to understand and reinvent helps with rapid growth as the approach would be customer-centric instead of it being driven by trends based on market competition.
Despite the common assumption that reading about entrepreneurship doesn't help you become one, it is important to read and understand experiences to avoid common mistakes and be exposed to different business models.
Of course, we are no Bill Gates who can read about 750 words per minute and follow that with a 90% retention rate but we sure can try!
It’s not uncommon to see nepotism in the Business world.
Even The President of the United States, Donald Trump took over his father’s company, and now, his sons run the Trump empire.
There are endless debates on how businesses run successfully for generations.
Though arguably, it’s a matter of convenience to pass on power to our kin, studies suggest that genetics could contribute a fair share to why they run successfully.
Here’s some complex math for you:
Behavior patterns = Complex
Genetics = Complex
Behavioral Genetics = ? (haha, complex math)
Behavioral Genetics is barely black and white.
It’s hard to figure out what shade of grey we are looking at (we might need Christian’s help on that one!).
Since behavior entails what you are and what you see, it involves a great deal of both environmental factors and multiple genes that contribute to one trait of ours.
In the recent past, there has been emerging research conducted on such grey areas of behavioral science.
Thanks to all the mass observations about business tycoons, entrepreneurship has been one such potential studied.
Most genetic research, to resolve debates of behavior, always conducts studies on twins.
Their high similarity in genetic makeup leads to more conclusive results than in general human studies.
Studies have shown that 30 to 35% of the entrepreneurial traits could be attributed to heritability.
Though this implies that environmental factors contribute to the rest of the major 70%, 1/3rd of the fraction is a significant number to make or break, in this fast-paced world.
Nonetheless, having a genetic predisposition only increases the likelihood of becoming a successful entrepreneur, but that has to coincide with various other environmental factors and maybe a few tik-tok videos to make it big in this world.
As organizational behavior is a higher-order function, genes that are related to it often are responsible for very brainy activities.
Brain activities control the release of different brain chemicals like neurotransmitters and these activities are controlled by different genes responsible for their action.
For example, Serotonin levels can contribute to the attitude of ‘taking chances’.
This would help you be less risk-averse which is beneficial for an entrepreneur.
As we are all humans and the genetic outline is pretty much the same, we often find different variations of one particular gene.
These range from the tiniest of a change at a nucleotide level (the fundamental unit of the DNA structure) called Single Nucleotide Polymorphisms (SNPs) to big structural variations where chunks of the DNA are cut out, duplicated, etc.
These are often causes of genetic diseases.
But SNPs are the most common type of variation known to human beings.
The outcome of the variations depends on the extent of its influence in the gene.
The functions of the gene could be altered, like structuring a protein or if it is a regulatory gene, it might affect that function.
Some of these variations could make us susceptible to different traits.
This applies in case of behavioral traits too.
Now, these different variations make us susceptible to traits that are common in successful entrepreneurs, it increases our likelihood of becoming one, too.
The likelihood increase would take place only with the possession of the uncommon variation, often referred to as the minor allele.
A major study conducted to understand the genetic influences in self-employment discovered SNPs in the gene RNF144B, indicating an increased probability of being self-employed.
The minor allele T, of an SNP in this gene, has an association with an increased probability of being self-employed.
| TT Genotype | Increased probability of being self-employed |
| CC Genotype | Normal entrepreneurship skills |
The SNPs of the SV2C gene was also part of the study with two different variations. RNF144B is a gene that codes for a structural protein.
SV2C on the other hand codes for brain transport proteins called synaptic vesicles. So the range of the involvement of these genes is extremely varied.
| AA Genotype | Increased probability of being self-employed |
| GG Genotype | Normal entrepreneurship skills |
Several other genes also have an association with entrepreneurship potential.
To quote an example from Scott Shane’s best-seller:
Born Entrepreneurs, Born Leaders: How Your Genes Affect Your Work Life
Some people might have a version of a gene that increases their odds of making large financial bets, but the influence of this gene on risk-taking might only be manifest in high-pressure, short-time-to-make-a-decision situations, such as currency trading operations.
Thus, the gene might not influence managers’ decisions to gamble billions of dollars on new technologies after months of careful evaluation, but it might affect traders’ choices to bet billions of dollars on currencies in a few seconds on foreign exchange markets.
This also helps us understand how there are no binaries with these behavioral traits.
However, the genetic predisposition only increases the likelihood of your entrepreneurship potential.
If the person who is good with big financial bets never explores a career in a Wall street set-up, he would never discover his potential.
The rest of the environmental factors HAVE to coincide to create a successful entrepreneur.
This could be as fundamental as having the means to source capital for the implementation of the business idea.
Entrepreneurship potential still has many unknowns we are yet to explore.
But we have to understand and acknowledge that various factors are contributing to an entrepreneur’s success.
Be it genetic or environmental, it is a life-long journey of being best at what you do.
Being successful in any field takes some serious perseverance and commitment.
So, regardless of the origin of our instincts, let’s try to be good at what we do!
Upload your raw data to Xcode Life for insights into 700+ health-related traits!
Our body is fueled everyday by different nutrients – some that are required in larger quantities while others in lesser, and few in traces amounts. Some nutrients form structural components of our cells whereas, there are others that participate or regulate various functions and processes in the body. One such trace mineral, and an essential one too, is copper.
Our body needs minerals for various physiological processes.
While some minerals are needed in larger quantities like sodium, calcium, and potassium, some like copper are essential trace minerals that are vital for survival.
Copper is found in all body cells and plays an important role in the formation of blood vessels, maintenance of the nervous, and the immune system.
Our body has about 2 mg of copper per kilogram of body mass.
Though copper is found in all parts of the body, organs like the liver, kidney, heart, and the brain have it in higher quantities.
As mentioned earlier, our body needs copper for plenty of activities. These include:
Intake of less than the Required Dietary Allowance (RDA) of copper can lead to copper deficiency whereas, taking in more than the RDA can lead to copper toxicity, both of which can be harmful.
For adolescents and adults, the RDA is about 900 mcg per day.
Any intake above 10,000 mcg or 10 mg per day can be toxic.
The copper requirement of the body changes with age, gender, and conditions like pregnancy.
| Age | Male | Female | Pregnancy | Lactation |
|---|---|---|---|---|
| 0-12 months | 200 mcg | 200 mcg | ||
| 1-3 years | 340 mcg | 340 mcg | ||
| 4-8 years | 440 mcg | 440 mcg | ||
| 9-13 years | 700 mcg | 700 mcg | ||
| 14-18 years | 890 mcg | 890 mcg | 1000mcg | 1000 mcg |
| 19+ years | 900 mcg | 900 mcg | 1300 mcg | 1300 mcg |
Copper deficiency can occur due to diet, nutritional deficiencies, or digestive issues resulting from surgeries or other conditions.
These are called acquired copper deficiencies.
Another type of copper deficiency is inherited copper deficiency that is genetic in origin.
Surgeries like bariatric surgery, gastrectomy, upper GI tract surgery, and other stomach surgeries result in copper deficiency.
Inherited copper deficiency is rare and affects one in every 1,00,000 births.
The gene causing this condition is inherited in an X-linked recessive manner and runs in families.
The SELENBP1 is located on chromosome 1 and is a part of the selenium-binding protein family.
Selenium is an essential mineral and is known for its anticarcinogenic properties and a deficiency of it can result in neurologic diseases.
The protein encoded by the SELENBP1 gene is said to play a selenium-dependent role a ubiquitination/deubiquitination-mediated protein degradation.
One of the phenotypes for the SELENNP1 gene is serum copper measurement.
The presence of the G allele in this SNP causes a decreased absorption of copper resulting in an increased risk of developing a copper deficiency.
The SMIM1 gene or Small Integral Member Protein 1 is located on chromosome 1 and codes for a small, conserved protein that takes in part in the formation of red blood cells.
The A allele of the SNP rs1175550 is associated with serum copper measurement.
The main problem with copper deficiency is that it is hard to diagnose as its symptoms are very similar to other nutritional deficiencies such as vitamin B12 deficiency.
Since low copper levels in the body can affect a person’s immunity, it is important to identify it in time.
Clinical symptoms of copper deficiency include:
Copper deficiency can also be recognized hematologically as it presents with a triad of anemia, neutropenia, and thrombocytopenia (rare).
Copper deficiency is usually not the first thing that is diagnosed when one presents with symptoms as many nutritional deficiencies present with similar clinical symptoms.
However, your doctor may suspect copper deficiency if you have a history of any of the following:
If your doctor suspects a copper deficiency, he/she may order a blood test for detecting plasma copper levels.
However, one must note that this is not a conclusive test for copper deficiency as many other factors can cause a false elevation of blood copper levels.
The first step in the treatment of copper deficiency is identifying the cause and removing or treating it.
For example, if the copper deficiency is due to excess zinc supplements, your doctor will reduce the zinc supplements to allow more absorption of copper.
Many a time, doctors prescribe copper supplements to make up for the deficiency of the mineral.
Common copper supplements include copper sulfate, copper gluconate, and copper chloride.
It can take about 4 to 12 weeks to treat a copper deficiency.
Taking 2 mg of copper per day can help restore normal copper levels in a deficient individual.
However, the exact dosage is determined by a doctor after evaluating other health and lifestyle factors.
In the case of individuals who cannot take oral copper supplements, they may be put on IV copper treatment.
Along with copper supplements, consuming copper-rich foods can really help.
Copper is an essential mineral for the body but it is also a trace mineral which means that our body needs a very little amount of copper to function.
However, many people suffer from a deficiency of this mineral that can result in complications over a period of time.
Some people who require copper supplements include:
However, care must be taken to consult with your doctor before taking copper supplements as copper toxicity can be as harmful to the body as copper deficiency.
Apart from this, people who have had surgery such as bariatric surgery, gastrectomy, or those who suffer from GI tract diseases such as IBS, celiac disease, etc., also need supplements as they are more likely to have copper deficiency due to the poor absorption.
There are certain rules to follow when taking copper supplements. We know that zinc interferes with copper supplements and so, avoid taking both zinc and copper supplements at the same time.
Fix two different times for both supplements and stick to these times every day.
Ideally, take your copper supplement at least two hours after taking your zinc supplements for maximum absorption.
Copper supplements can cause stomach irritation and acidity, and hence, copper supplements can be taken with meals can help reduce irritation.
Many people who take antacids may need higher dosages of copper supplements as antacids interfere with the absorption of copper.
Copper supplements can cause side effects and the common ones are:
There are symptoms of overdose that one must watch out for and avoid:-
Apart from supplements, diet plays an important role in restoring normal copper levels in the body.
To treat copper deficiency and maintain optimum copper levels in the body, some copper-rich foods that you can include in your diet are:
Upload your raw data to Xcode Life for insights into 700+ health-related traits!
https://ods.od.nih.gov/factsheets/Copper-HealthProfessional/#en3
https://www.genecards.org/cgi-bin/carddisp.pl?gene=SELENBP1
https://www.snpedia.com/index.php/Rs2769264
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3766178/
https://www.genecards.org/cgi-bin/carddisp.pl?gene=SMIM1&keywords=SMIM1
Ever wondered how going off carbs for a couple of days almost always shows instant results? Thank all the glycogen stored in your body. But some people have trouble storing this entity as we do, disrupting their chance to live a typical life. Let’s peak into what actually happens with Glycogen Storage Disease.
Metabolism is a biological process that breaks down the food we eat and provides energy to keep us alive.
In some cases, different key stakeholders in this process fail to fulfill their duty.
There is a spectrum of conditions that fall under the umbrella of Glycogen Storage Disease (GSD), which cause such trouble.
Since it did not have any popular awareness challenge go viral (bring back the ice buckets!) and fortunately is a rare condition, it hasn’t had too much light thrown on it.
According to the reports, the incidence rates appear to be 1 in 100,000.
As the symptoms set out at an early age, Glycogen Storage Disease appears to affect the little ones more than the adults.

Our body uses glycogen, a complex sugar compound, as a fundamental storing unit of energy. Metabolizing glycogen, to break it down into glucose, provides the instant energy we need. As we need to conserve some of this energy, these glucose molecules are combined back into glycogen. This is used as a reservoir to tap into when there is a lack of energy supply. Different parts of the muscles and the liver act as storage units for glycogen.
For this process to take place, some special proteins called enzymes (biocatalysts) aid the formation and deformation of glycogen.
When these enzymes don't function optimally, it leads to a spectrum of diseases.
This could lead to a range of different symptoms depending on the type of diseases.
The types are classified based on the enzyme which is at fault. It starts from GSD1 and runs up until GSD 15.
The types 1 to 4 cover almost 90% of the reported cases, with sub-type of GSD1 - GSD 1a, aka Von Gierke Disease being most common.
As the condition affects the necessity of food metabolism, symptoms start to show 3 to 4 months after birth.
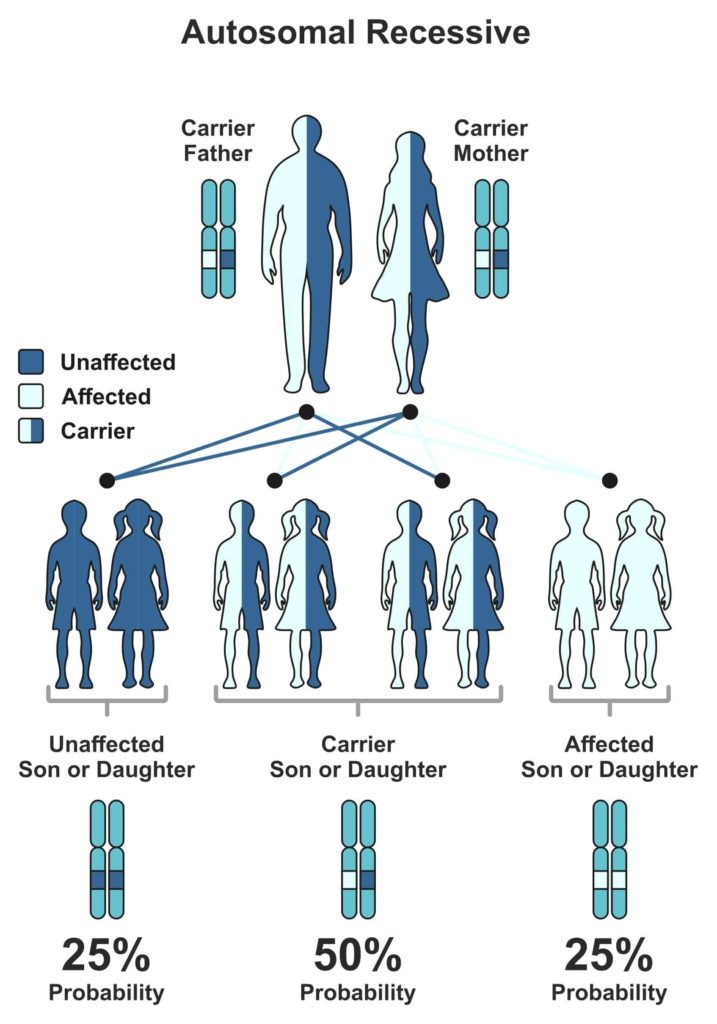
The cause of Glycogen Storage Disease is genetic.
The gene that is responsible for the malfunction of the enzyme can pass on from the parent generation to the next, making it hereditary.
But the child will express symptoms of the associated GSD, only when both parents possess a defective gene.
Every human gets their 23 chromosomes from each parent.
Genes that are subunits to chromosomes have one trait, which is dominant and other recessive (some exceptions, of course).
The level of expression marks the difference between them.
Now, for the expression of a recessive trait, both parents must pass on their recessive versions of traits.
The Mendelian world calls this an autosomal recessive condition.
A random process selects the gene to be passed down to the next generation.
In the case of autosomal recessive conditions, there is a 25% chance of occurrence.
If just one parent passes it on, then the child will remain healthy but acts as a carrier of the gene.
Carriers could potentially pass it on to the coming generations.
We obtain glucose from the diet we eat.
Glycogenin is an enzyme that is responsible for cutting down this glucose into short fragments.
Another enzyme, glycogen synthase, helps in the conversion of glucose into Glycogen.
Now, some branching enzymes add branches to Glycogen, which the liver then stores as a reservoir of energy.
When we fast or there is a need for muscle contraction, the body taps into the said reservoir.
The process of breakdown involves four enzymes.
Glycogen Phosphorylase and glycogen debranching enzymes help in unraveling the molecule to release glucose and expend energy.
Another method of breaking it down involves enzymes such as a-glucosidase and Glucose-6-phosphatase.
Every action in our body is instructed by the beautifully wound helix, DNA.
As these enzymes correspond to specific genes, any defect in this gene will directly translate into the enzyme’s action.
Take the example of the most common type of GSD - GSD type 1a.
One of the enzyme genes involved in breaking down glycogen is Glucose-6-phosphatase. G6PC and SLC37A4 genes code for this enzyme.
As genes code for proteins and proteins like enzymes carry out the function, an error in the gene structure or function will lead to a collapse of the entire system.
A good analogy would be a loose brick in a building that could make it fall into pieces. Geneticists call these errors, mutations. As these ‘errors’ have been major contributors in the history of evolution, they have been beneficial in many ways.
Unfortunately, not in the case of Glycogen Storage Diseases.
So, when there is a mutation in this gene, glucose-6-phosphatase does not play its role and leads to the build-up of Glycogen and fat.
We know, too much of anything is toxic. Hence, the accumulation of Glycogen and fat hinders the function of organs like liver and kidney.
In the case of type 3 Cori disease/Forbes disease, a distinct part of the gene, called Exon3, carries two mutations that cause the debranching enzyme to malfunction.
As a debranching enzyme is responsible for the decomposition of Glycogen, it leads to toxic accumulation.
Andersen disease (type 4) affects the GBE1 gene that codes for glycogen branching enzyme leading to large amounts of abnormal Glycogen accumulated, causing severe conditions like liver cirrhosis, which is ‘doctor’ for scarring.
Types 1, 3, and 4 are far more common in comparison to other types.
Most often, all different types have a combination of some common symptoms in varying intensities.
As the age of onset is rather young in the case of Glycogen Storage Diseases, doctors generally ask the parents about symptoms showcased by their child and call for relevant tests.
Blood tests and MRI/ultrasound scans are routine. In some cases, a biopsy of a suspected organ might be required for confirmatory diagnosis.
Genetic testing has evolved over time and is performed to confirm the diagnosis.
This is extremely helpful in the case of couples who have observed a family history of Glycogen Storage Disease.
Seeking genetic counseling before planning a family will help provide a clearer picture of the chance of occurrence in their case.
Carrier testing for at-risk family members and prenatal diagnosis have led to significant changes in family planning.
The treatment options are specific to the type of GSD diagnosed with the patient.
Generally, it includes major dietary restrictions.
Uncooked corn starch can be a good feed to children over two years of age, as corn starch can promise a slow release of glucose.
This is fed in small portions throughout the day.
For type 1, elimination of food which is high in lactose and fructose is advised (that's pretty much everything tasty, from mozzarella to maple syrup).
Allopurinol is prescribed if there is a risk of kidney stones or gout, as it reduces the levels of uric acid in the blood.
Some extreme cases like the type 4 of GSD could require liver transplant depending on the extent of the condition.
When the patient is prone to frequent muscle cramps during exercise, a high protein diet is advised.
In some cases, the intake of glucose and fructose is advised. And of course, as their muscles are now more susceptible to damage, over-exhausting the body is a big No-No.
Unfortunately, prevention is barely an option.
As this is a genetic condition, the only way of prevention is to ‘not pass on the genes’.
Parents can seek genetic counseling to check if both carry the defective gene as it takes two to tango in this case.
But we have come a long way with the prognosis of the condition.
The unawareness of the disease’s details led medical researchers to believe GSD to be a fatal condition until the early ’70s.
People now live long and normal lives with significant dietary shifts.
This barely seems like a change in the millennial world of Keto and Atkins!
Speaking of Keto and Atkins, Glycogen is the secret quarterback in the low-carb diet game.
Glycogen storage and weight loss have a strange love story.
A typical healthy liver in an individual can hold up to 400 grams of glycogen and muscle cells, about 100 grams.
As glycogen and water co-exist in a 1:3 ratio, there are 3 grams of water present for every gram of glycogen.
This is the real reason behind the initial weight loss observed when any sort of low-carb diet is practiced.
It would rather be ideal for comparing body fat percentage or keeping track of monthly weight changes, for getting a better measure of body change as opposed to this initial quick loss of weight.
The body stores about 1500-2000 calories of Glycogen typically.
With a low-carb diet, the body uses this up and has little or no reservoir of energy. Possibly dehydrated.
This can lead to a constant state of fatigue in some extreme cases that could potentially damage the liver as it would be exposed to undue stress.
So we should be cautious when we make such lifestyle changes and always seek professional guidance.
In the case of sportsmen, a low-carb diet could lead to quick use of the stored Glycogen, especially the ones stored in the muscles.
This leads to a case of muscle fatigue and, in extreme cases, will lead to a phenomenon known as “hitting the wall”. Glycogen is also brain food.
So severe lack of Glycogen leads to cognitive symptoms like confusion, disorientation when you have a “bonk” during exercise.
Though there is cutting current edge research to discover new enzyme replacement therapies and gene therapies, this spectrum of diseases affects many lives.
But once again, we are hopeful that genomics will save the day!
Upload your DNA raw data to Xcode Life for insights into 700+ health-related traits
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4146814/ - Ozen H. (2007). Glycogen storage diseases: new perspectives. World journal of gastroenterology, 13(18), 2541–2553. https://doi.org/10.3748/wjg.v13.i18.2541
https://www.tandfonline.com/doi/full/10.3109/01913123.2011.601404 - Hicks J, Wartchow E, Mierau G. Glycogen storage diseases: a brief review and update on clinical features, genetic abnormalities, pathologic features, and treatment. Ultrastruct Pathol. 2011;35(5):183‐196. doi:10.3109/01913123.2011.601404
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(04)16986-9/fulltext Astrup, A., Meinert Larsen, T., & Harper, A. (2004). Atkins and other low-carbohydrate diets: hoax or an effective tool for weight loss?. Lancet (London, England), 364(9437), 897–899. https://doi.org/10.1016/S0140-6736(04)16986-9
https://onlinelibrary.wiley.com/doi/abs/10.1038/icb.2015.109 - Gleeson M. (2016). Immunological aspects of sport nutrition. Immunology and cell biology, 94(2), 117–123. https://doi.org/10.1038/icb.2015.109
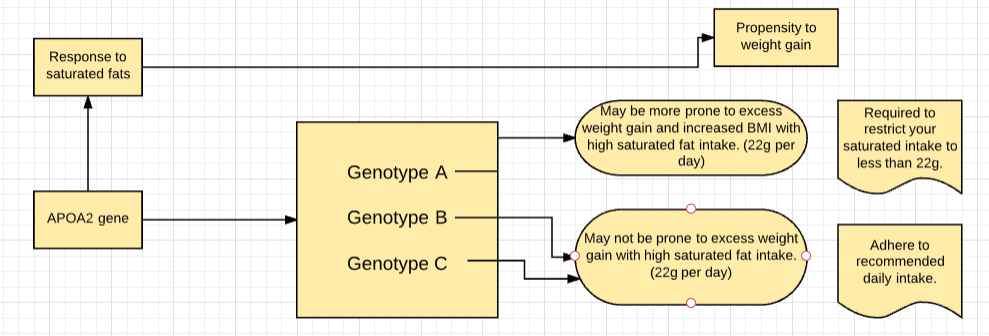
Our genes are a template for how our bodies work. Most people on keto diets tend to consume a high amount of saturated fats. The diet works only when the stored fat is properly broken down and used for energy. Certain variants of the APOA2 gene tend to interfere with this saturated fats metabolism and hence, carriers of such variants may not get the desired benefit from this diet.
There seems to be an endless debate about whether saturated fats are good or bad for your health.
The truth is, all of us need a little bit of fat for some body functions like hormone production or maintenance of cell integrity.
But, what is considered 'too much' for your body is determined by certain gene variants you carry.
Let's explore this concept with a diet that's been constantly gaining popularity for weight loss and prevention and treatment of certain health conditions:
The basis of this diet is ketosis, which refers to the metabolic process in which the body converts stored fats into energy, releasing ketones in the process.
Hence, the conventional keto diet, which calls for high consumption of fats may work only if the stored fat is metabolized efficiently.
Several genes contribute to how your body reacts to saturated fats.
APOA2 gene is one of them that determines how well you tolerate saturated fats and how well you can transport cholesterol.
Depending on the variant of this gene you carry, you may need to modify the keto diet a little bit, in order to maximize its benefits to your body.
From the evolutionary perspective, certain human societies, such as those in the colder northern regions are likely to have subsisted on the large intake of fats for hundreds of generations.
As a result, they could have developed adaptations that enable them to metabolize this macro ingredient in food quite efficiently.
If you have inherited those genes, then your body is better able to cope with fats intake.
APOA2 gene produces a protein apolipoprotein -II, which plays a role in fat metabolism and obesity.
Individuals with the sensitive variant of this gene are more prone to increased BMI (6.8 times greater BMI), waist circumference, and body weight in response to high levels of saturated fat (more than 22g of saturated fats per day).
This was an observation in comparison to the people with the non-sensitive variant of the gene consuming the same amount of saturated fats.
It is vital for the carriers of the sensitive variant to limit their saturated fat intake.
However, there was no difference among individuals with both versions, in terms of weight and BMI when saturated fat intake was low (less than 22g per day).
One possible mechanism that could help explain the above gene-diet interactions is that, the sensitive variant of this gene produces lower levels of the protein, APOA2 (regulates the satiety response), resulting in low satiety and greater appetite among individuals with higher saturated fat intake.
This appetite may preferably be for foods rich in saturated fat and this higher fat intake would lead to greater weight.
Other genes like FTO, PPARG also impact the metabolism of saturated fats.
Carrying even 2-3 variants that affect saturated fats metabolism can pose a challenge to cholesterol control and weight loss.
It is thus vital for such individuals to alter their diet with lesser intake of saturated fatty acids.
Replacing saturated fatty acids with monounsaturated fatty acids (MUFA) and poly-unsaturated fatty acids can be a good start.
Sources of MUFA
Sources of PUFA
Upload your DNA raw data to Xcode Life to know your genetic variants for saturated fat metabolism.
25% to 50% of people who reported to hospitals in China with coronavirus in December 2019, had hypertension or other comorbidities like diabetes, cancer, or heart conditions. In Italy, 75% of COVID-related deaths included hypertensives. Hypertension and severe COVID symptoms have a genetic connection. But how interlinked are they? Read on to find out more!
The clinical and epidemiological features of COVID-19 have been under constant study and several research studies have been published about it over the last several weeks.
A lot of focus is on the comorbidities that have an association with COVID, in particular.
The most common comorbidities in one report were hypertension (30%), diabetes (19%), and coronary heart disease (8%).
ACE inhibitors, which are used to treat hypertension, have been researched to increase the ACE2 receptor expression, to which the coronavirus binds to.
But, it is important to note that none of these can be declared as a 'cause' of COVID since these are more prevalent in the elders, who appear to be at an increased risk for COVID.
However, blood pressure control is extremely important to reduce the impact of COVID in your body.
The coronavirus appears to affect any individual despite factors like their age or gender.
However, recent research reveals that some people tend to have more severe symptoms, in comparison to others who may experience mild symptoms or be completely asymptomatic.
Some genetic factors tend to influence how the virus enters your body, and consequently, how the virus affects you as well.
There is a wide acceptance amongst the scientific community that there is a genetic risk factor that causes severe symptoms in some individuals, while rendering other asymptomatic.
One such disease that scientists have researched is hypertension.
The limited studies on this reveal that the novel coronavirus latches on to the human protein ACE2 receptors and gains entry into the lungs.
Hypertensive individuals are prescribed Angiotensin-Converting Enzyme(ACE) inhibitors, and some studies have shown that these medications increase the number of ACE receptors, thereby increasing the portals for entry of the virus.
There are, however, opposing theories with a few groups of scientists saying that the ACE2 can actually protect the lungs from a very severe infection of 2019- nCov.
A very common health condition that is prevalent today is hypertension or abnormally high blood pressure.
A blood pressure level of 120/80mm Hg is considered normal, and having blood pressure equal to or higher than 130/80 mm Hg is called hypertension, in an otherwise healthy individual.
Though a common condition today, hypertension runs in families, and therefore, genetics and heredity may play a major role in determining the disease risk.
Individuals who have hypertensive parents tend to have an increased risk of developing the condition. However, how the exact inheritance of this condition is still unknown.
Many Genome-Wide studies have been conducted to study the influence of genes on the development of hypertension.
Around 280 genetic variants have been found that are said to increase the risk of hypertension and other associated conditions such as coronary artery disease.
Some genes that have a significant role to play in the development of hypertension are –
With the currently available studies, it has been observed that there are many genes that play a role in the pathophysiology of hypertension. It is highly unlikely that just one or two will emerge as the leading genes associated with the condition.
Now it is as simple as just following 3 simple steps to identify your risk for hypertension using your DNA raw data.
So far, it is quite evident that hypertension is high-risk comorbidity that results in severe symptoms if affected by COVID.
Pneumonia is one of the most common complications in severe cases.
In a hypertensive individual, high blood pressure damages the blood vessels and arteries. Therefore, it results in reduced blood flow to the heart.
As a result, your heart needs to work extra hard to pump blood, so it reaches all parts of your body.
When this happens over a period of time, it results in the weakening of the heart muscles.
The same effect can occur when there is hypercholesterinemia occurs together with hypertension.
Most common symptoms to look out for if you suspect a COVID infection include:
As a hypertensive individual, you need to take extra care to reduce your chances of contracting COVID. Here are some guidelines that you need to follow:
https://www.cebm.net/covid-19/coronaviruses-a-general-introduction/
https://academic.oup.com/eurheartj/article/38/29/2309/3852720
https://jasn.asnjournals.org/content/13/suppl_3/S155
https://academic.oup.com/ajh/article/33/5/373/5816609
https://pubmed.ncbi.nlm.nih.gov/24842388/
Upload your DNA raw data to Xcode Life to know your genetic predisposition to hypertension.
Diabetes is a chronic disorder wherein the body no longer responds to insulin. The disease could reduce the efficiency of the body’s immune system. As such, diabetes is a common comorbidity of COVID-19, with up to 20% of patients requiring intensive medical care. With lockdowns and social restrictions in place across the globe, here are some ways in which you can protect yourself from the novel coronavirus.
The current COVID-19 pandemic has affected all our lives in one way or another. The cases report a range of symptoms from mild or asymptomatic cases to severe forms of pneumonia that could lead to the patient’s death.
With newer evidence released on a daily and monthly basis, researchers worldwide are trying to deduce the infection pattern, characteristic symptoms, potential treatment patterns, and drugs.
COVID-19 is an infection of a new coronavirus called the SARS-CoV-2 that emerged in the Wuhan region in China. This disease was so widely spread, that the World Health Organisation declared a global pandemic in March 2020.
The SARS-CoV-2 is a type of coronavirus, which falls under the same family as SARS and MERS. Some experiments have hypothesized that the virus has some affinity to angiotensin-converting enzyme receptor 2 (ACE2), which acts as the gateway to the human body.
As many scientists rush to find the cure for the disease, a pressing question remains- why is there such a disparity between patients of COVID-19? How are there some individuals showing absolutely no symptoms, and on the other hand, why are some patients exhibiting severe pneumonia-like symptoms?
The known factors, like age and previous medical history, makes an individual more susceptible to showing severe symptoms.
However, there are cases of perfectly healthy young people showing severe symptoms as well. Some underlying genetic factors can be responsible for this.
As mentioned above, one hypothesized path that the virus takes to the body is through latching onto the ACE2 receptor.
Scientists have found variants of the gene that codes for ACE2, which could influence how the protein functions or impact the structure. This, in turn, affects how the virus could infect a person.
Another factor that could influence how the virus infects an individual could be the person’s blood group.
The ABO gene determines the blood type of a person and could shine a light on how susceptible a person is to the virus.
Both these genes are from preliminary studies, and this needs more validation and a larger group of volunteers to conclude any observation.
Diabetes is a condition in which there is an impairment in the body’s ability to produce or respond to insulin.
This results in abnormal levels of carbohydrates and elevated levels of glucose in the blood.
People with diabetes are at an increased risk, as they have an impaired immune response to infection.
This applies to both cytokine profiles and activation of T-cells and macrophages.
The impact of having an impaired response to insulin affects the body’s response to viral infection and potential secondary infection in the lungs.
A study compared hospitalization rates of COVID-19 patients and the underlying medical conditions.
Of all the volunteers in the study, 7% were hospitalized and admitted in the ICU, and 77% were not hospitalized. While analyzing the patients with diabetes, up to 20% were hospitalized, and only 45% were not hospitalized.
This data shows that patients with diabetes require extra medical attention if diagnosed with COVID-19.
Patients with type 2 diabetes are also at risk of being obese. This is an additional risk factor for severe infection.
In the case of the 2009 H1N1 epidemic, about twofold more patients diagnosed with the disease, with a history of obesity, ended in ICU, and took longer to recover.
Finally, the most common co-morbidities to COVID-19 are hypertension and diabetes.
These diseases are both treated with ACE2 inhibitors.
This means that a patient with an ACE inhibitor would have an increased expression of ACE2.
Since the novel coronavirus targets ACE2, it could facilitate COVID-19 infection, and place these patients at a high risk of disease and fatality.
Genetics plays a role in type 2 diabetes; however, factors like lifestyle choices play a larger role in the manifestation of this disease.
A choice for healthy living can heavily lower the chances of developing type 2 diabetes.
This includes staying healthy by maintaining a healthy weight and choosing healthy foods.
It is possible to test for your genetic predisposition towards diabetes using your 23andMe DNA raw data.
If you have are a diabetic/ have a predisposition to diabetes, it is important to be prepared. Some measures that you can take are:
There are three main pillars of diabetes maintenance, monitoring, exercise, and diet. Measures that you can take with respect to exercise and monitoring are explained above, and the following details a diet plan that you can follow.
COVID-19 is caused by a novel coronavirus, SARS-CoV-2. The symptoms and the path of infection are still being studied, with new data being released on a daily basis. Individuals with comorbidities, especially like diabetes and hypertension, must strictly follow social distancing practices. If they do step out, measures of wearing a face mask, carrying a sanitizer, and washing hands thoroughly with soap can help prevent infection.
Could genetics play a role in the severity of COVID-19?
COVID-19 Infection in People with Diabetes
Upload your DNA raw data to Xcode Life to know your genetic predisposition to diabetes.
Carbohydrates are one of the main classes of food. It is the main source of energy for the body. They are a group of organic compounds present in the form of food in cellulose, starch, and sugar. They are called carbohydrates, as they contain hydrogen and oxygen in the same ratio as water (2:1). These are then broken down to release energy.
Due to the association of carbohydrates with weight gain, the carbs may disguise as an enemy to a healthy diet. However, the right kind of carbs in the right amounts can definitely earn a rightful place in your diet.
A healthy weight is an important element of good health. The amount of food you eat and what you eat is important for maintaining a healthy weight.
For years, there was a myth that a low-carb diet is the best way to lose weight, but a growing body of evidence suggests otherwise.
Carbs are sub-divided into three categories depending on the number of sugars present and the nature of the chemical bonds between them.
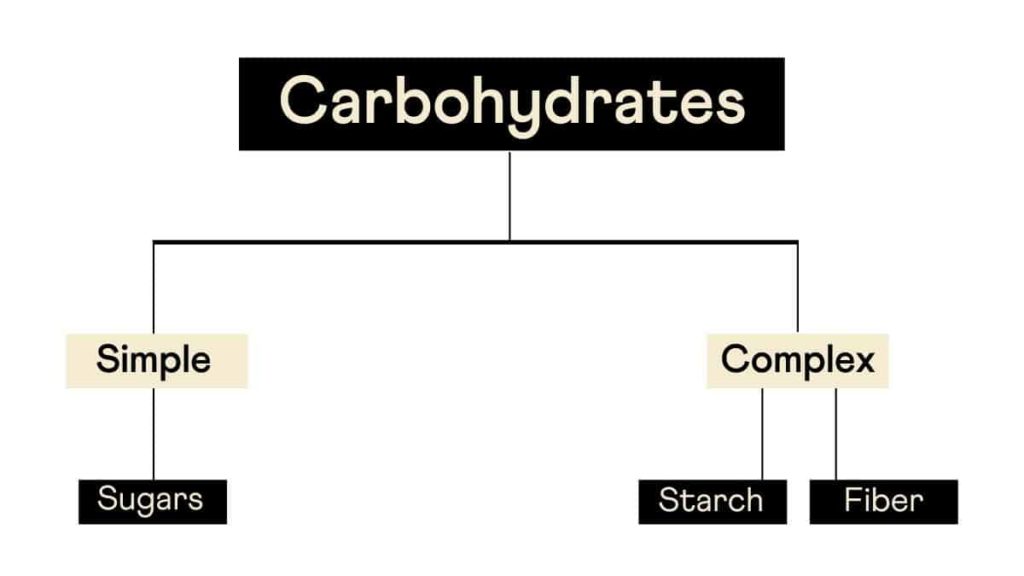
Although this is the conventional way of classifying carbs, a more pragmatic approach would be to classify them as refined and whole carbs.
Whole carbs include vegetables, legumes, whole fruits, and grains, which are unprocessed and thus have their nutrient content intact.
The stripping of nutrients in refined carbs as a part of processing makes them count as 'empty calories.'
This removal of the nutrients results in rapid absorption and metabolism of these carbohydrates.
This results in spiked sugar levels and unstable energy levels, the latter of which causes “sugar rush” after consuming sugar-rich foods.
The refined or the sugary carbs are simple carbohydrates that the body quickly absorbs.
Their metabolism occurs rapidly, which results in major swings in the blood glucose levels. This induces hormonal and metabolic changes that can promote overeating.
Not all carbohydrates are bad for health.
Unprocessed carbs that are present in vegetables, fruits, and grains are healthy.
Studies reveal that these improve metabolization and help in weight loss.
Another class of carbs, the processed ones, are unhealthy because they lose the fiber during processing and contain no essential nutrients.
Examples of these include white bread, white rice, and the like.
Intake of foods containing processed carbs can result in weight gain and increased risk of type 2 diabetes.
Studies show that high unprocessed carbs in the diet can lead to a craving for more carbs, and people tend to get caught in the vicious cycle.
Thus, making changes to your diet by including more of unprocessed carbs can be a healthy choice.
Studies have shown that there is a link between genetic factors and dietary factors such as weight loss, weight gain, obesity.
Nearly 70% of the world population carries the gene for obesity. This explains why obesity is growing rapidly around the world.
However, people can reverse this gene's effect by exercising and including more protein in their diet.
A study has found an association between the FTO gene and the intake of carbohydrates.
The individuals with the A variant were found to have a higher risk of obesity than ones with the CC wild type.
The FTO gene has a negative association with over-eating.
About 23% of the global population carries a variant in the AMY1 gene, which shows an association with low copy numbers of the gene and reduced ability to digest starch.
70% of people from agricultural populations have an AMY1 copy number variant, which shows an association with better starch digestion and lower risk of obesity when compared to 37% of non-agricultural populations.
The conventional diet plans and workout regimes architected for weight loss need not help everyone achieve their desired goals.
There is a multitude of factors that influence weight loss, including a person’s lifestyle, genetic makeup, and the environment.
Your genes can influence how you metabolize the nutrients you get from your diet. This directly has a role to play in weight gain/loss.
For instance, some people may possess a genetic variant that aids in the faster metabolization of carbohydrates, while others may carry a variant that will help in faster break-down of saturated fats.
You can leverage such genetic information to adopt a practical and personalized weight loss plan.
While genetic tests may not lay out the A-Z of weight loss, it certainly helps you pin the right path for your weight loss journey.
Upload your DNA raw data to Xcode Life for insights into 700+ health-related traits
CYP1A2 codes for the production of 21-hydroxylase, which is part of the cytochrome P450 family of enzymes.
This family of enzymes is quite important as it is a part of many processes, that include breaking down drugs, production of cholesterol, hormones, and fats.
The adrenal glands secrete the enzyme, 21-hydroxylase.
Situated on the top of the kidneys, the adrenal glands also produce hormones like epinephrine and cortisol.
Incidentally, 21-hydroxylase plays a role in the production of cortisol and another hormone named aldosterone.
Cortisol is a stress-related hormone and plays a role in protecting the body from stress, as well as reducing inflammation.
Cortisol also helps in maintaining blood sugar levels.
Aldosterone, also known as the salt-retaining hormone, regulates the amount of salt retained in the kidneys.
This has a direct consequence on blood pressure, as well as fluid retention in the body.
There seems to be an interesting trend in the activity of the CYP1A2 gene and caffeine intake.
The consequence of being a “rapid” or a “slow” metabolizer of caffeine can have effects on an individual’s cardiovascular health.
This article explains the wide-ranging effects of this gene, caffeine intake, cardiovascular health, hypertension, and even pregnancy!
In the body, CYP1A2 accounts for around 95% of caffeine metabolism.
The enzyme efficiency varies between individuals.
A homozygous, that is, AA genotype represents individuals that can rapidly metabolize caffeine.
Some individuals have a mutation in this locus and thus have the AC genotype.
These individuals are “slow” caffeine metabolizers.
There seems to be a link between CYP1A2, the incidence of myocardial infarction (MI), and coffee intake.
The positive effects of coffee include lowering a feeling of tiredness and increasing alertness; however, it can also narrow the blood vessels.
This increases blood pressure and could lead to cardiovascular disease risk.
Rapid metabolizers of coffee have the AA genotype and may unravel the protective effects of caffeine in the system.
However, the individuals that are slow metabolizers have a higher risk of MI.
This suggests that the intake of caffeine has some role in this association.
Yet another study associated DNA damage due to mutagens found in tobacco smoking could contribute to MI.
The study included participants who were genotyped at the CYP1A2 gene.
They found a group of ‘highly inducible’ subjects that had a CYP1A2*1A/*1A genotype.
These individuals have a greater risk for MI, independent of their smoking status.
This also means that there is some intermediary substrate that the CYP1A2 gene decomposes, and if this gene has a mutation, it could lead to a higher risk of MI.
In a study conducted on 2014 people, people who were slow metabolizers of caffeine (C variant) and who consumed more than 3 cups of coffee per day had an association with increased risk for myocardial infarction.
In a similar study on 513 people, increased intake of coffee, among slow metabolizers, has an association with an increased risk for hypertension.
Smoking is capable of inducing the CYP1A2 enzyme. Smokers exhibit increased activity of this enzyme.
In a study conducted on 16719 people, people with the A variant, and who were non-smokers, were 35% less likely to be hypertensive than people with the C variant.
In the same study, CYP1A2 activity had a negative association with blood pressure among ex-smokers.
But for people who were still smoking, the same gene expressed an association with increased blood pressure.
The gene CYP1A2 also has an association with caffeine metabolism and smoking.
A study aimed to tie these concepts together to find the relationship between this gene and blood pressure (BP).
The main measurements of the study were caffeine intake, BP, and the activity of the CYP1A2 gene.
In non-smokers, CYP1A2 variants (having either a CC, AC, or AA genotype) were associated with hypertension.
Higher CYP1A2 activity was associated with people who quit smoking and had lower BP compared to the rest but had a higher BP while smoking.
In non-smokers, CYP1A2 variants (having either a CC, AC or AA genotype) were associated with high caffeine intake, and also had low BP.
This means that caffeine intake plays some role in protecting non-smokers from hypertension, by inducing CYP1A2.
The intake of caffeine during pregnancy has an association with the risk of reduced fetal growth.
High caffeine intake shows a link to decreased birth weight.
The babies are also at risk of being too small during the time of pregnancy.
This was also observed in a study conducted on 415 Japanese women.
Women with the A variant who drank more than 300 mg of coffee per day were shown to be at an increased risk of giving birth to babies with low birth weight.
In conclusion, there are a lot of effects that the CYP1A2 gene has on the body. Many studies, as noted above, seem to link the activity of this gene to caffeine intake.
A variant at the CYP1A2 gene can determine whether an individual is a fast or slow metabolizer of caffeine, and this has some effect on the blood pressure and cardiovascular health of an individual.
The gene also plays a role in regulating an infant’s weight during the pregnancy of a woman, and this has a link with caffeine intake. It is thus interesting to analyze the effect of the variants of the CYP1A2 gene on an individual, based on their caffeine intake.
Upload it to Xcode Life to know about your CYP1A2 caffeine metabolism and caffeine sensitivity variants.
In the US, around 4.6 percent of the population aged 12 and above are diagnosed with hypothyroidism. It is a condition where the body does not produce enough thyroid hormones. The thyroid is an important regulator for many functions in the body. This butterfly-shaped organ controls blood pressure and, therefore, the efficiency of the digestive system. Since this hormone controls such important processes, it indirectly controls energy regulation and metabolism. Hypothyroidism can be diagnosed through routine blood tests, or after symptoms start to show. The most common cause of this condition is a disease called Hashimoto's.
Since the thyroid hormones are involved in so many functions, there may be many symptoms, and they may be wide-ranging and diverse.
The main symptoms are fatigue, cold intolerance, joint, and muscle pain. The other signs and symptoms are:
If left untreated, this could manifest into more severe symptoms like:
It has been a long-known fact that there is a complex relationship between thyroid, body weight, and metabolism.
Metabolism, determined by measuring the oxygen usage by the body over a specific time, is regulated by the thyroid hormone.
This measurement, when done in rest, accounts for something called ‘basal metabolic rate’ or BMR.
A low BMR may have an association with weight gain in certain cases.
Low thyroid hormone levels is a contributor to low BMR levels, and earlier, this was one of the diagnostic tools for hypothyroidism.
However, a low BMR could be due to an n number of reasons, and thus, it is not an effective measure of diagnosis anymore.
In the case of hypothyroidism, weight gain need not always be due to excess fat in the body.
Accumulation of salt and water being the contributor to weight gain is more plausible here.
Weight gain also depends a lot on the severity of hypothyroidism. In other words, more weight gain may be seen in cases of severe hypothyroidism.
To conclude, if weight gain is the only visible symptom, it’s better to explore the other contributors first before suspecting hypothyroidism.
Firstly, it is important to assess whether you’re at risk for the disorder, for quick diagnosis and treatment.
Early detection and treatment can help manage the complications that emerge if hypothyroidism is left untreated.
Identifying the risk factors also can point in the right direction for losing weight with hypothyroidism.
The TSHR (Thyroid Stimulating Hormone (TSH) Receptor) gene codes for a receptor protein that is found on the membrane of the cells that span across the thyroid gland.
The receptor binds specifically to TSH and plays a pivotal role in thyroid hormone metabolism.
A part of the receptor is outside the thyroid gland cell, and the rest remains in the cell.
The thyroid-stimulating hormone binds to the receptor, which brings about a series of reactions that control the development of the thyroid gland.
TSHR gene mutations can cause congenital hypothyroidism. These mutations change the building blocks that make up the receptor protein.
Moreover, the mutations affect the spread of the receptors across the thyroid gland. Other mutations make the receptors reside completely within the cell or impair the hormone's ability to bind with the receptor.
In conclusion, these mutations don’t allow the receptor to interact with the hormone efficiently.
When the receptor is unable to interact with the hormone, the hormone production is not stimulated.
This makes the body compensate for the lack of stimulation.
The gland either overproduces the hormone, and functions as normal, or severely under produces the hormone, causing hypothyroidism.
Mutations in the TSH receptor gene result in resistance to TSH, and therefore, a reduction in thyroid hormone production.
Mutations in TSHR may also cause thyroid hypoplasia, that is, an underdevelopment of the thyroid organ.
Firstly, the patient is assessed for symptoms like fatigue, dry skin, constipation, and weight gain.
Above all, the family's and the individual's medical histories are assessed for any previous condition like goiter or any other thyroid problem.
There are increasing reports that correlate the prevalence of thyroid autoimmunity and glycogen storage disease (GSD).
GSD is a condition where stored glucose reserves (stored as glycogen) cannot be degraded efficiently in the body.
Blood tests are the easiest way to diagnose hypothyroidism.
Usually, the levels of TSH and thyroxine are checked.
An underactive thyroid gland would produce high levels of TSH and low levels of thyroxine.
This is because the body is putting in extra efforts to produce the thyroid hormone.
The most common way to treat this condition involves the use of a synthetic thyroid hormone, levothyroxine.
This is an oral medication that reverses the signs and symptoms of the disorder.
Six to eight weeks after the medication, doctors recheck the TSH levels.
Excessive amounts of the hormone can cause increased appetite, insomnia, heart palpitations, and shakiness.
Other medication that you’re taking, as it can affect how the synthetic hormone work, and therefore, it is important to mention them.
This includes diabetes, antidepressants, estrogen, warfarin, heart medication, and supplements like magnesium, aluminum, iron, or soy.
Other treatments include diet supplements, surgery, and herbal remedies.
With regard to diet, it is important to note that conventional weight loss diets need not help in losing weight with hypothyroidism.
Make sure you eat the correct amount of calories that match your BMR as well as your physical activity levels.
Eating too little can slow down metabolism to the extent that any weight loss effort would be sabotaged.
Try to stick to a consistent meal plan and preferably stick to small but frequent meals.
Calorie counting, or keeping a food journal would help in understanding what foods you tend to eat more of, and this can provide an overview of your diet.
Thyroid patients experience tend to constipation and slow metabolism. So losing weight with hypothyroidism can be challenging.
Typically, diets consist of fiber-rich foods to aid in weight loss.
The following have a significant impact on the diet of a thyroid patient:
These components are essential in maintaining an anti-inflammatory diet.
This helps to calm the immune system and reduce excessive inflammation.
This diet also reduces the pressure on the liver and allows the body to metabolize the nutrients efficiently.
Although an underactive thyroid gland is associated with significant weight gain, treating the root cause with supplementing synthetic thyroid hormones does not aid in significant weight loss in patients.
In a study conducted by the American Thyroid Association, the synthetic thyroid hormone, levothyroxine, aided in losing weight in only half the volunteers with hypothyroidism.
The basis for natural remedies for hypothyroidism includes focusing on a balanced diet, curbing stress, and incorporate missing nutrients.
An optimal diet plan for patients with hypothyroidism has been explained in the section above.
Other supplements that can be added are as follows:
Low thyroid hormones affect the body's vitamin B levels.
Taking vitamin B supplements can help tackle the fatigue that the body faces.
Foods that are rich in this vitamin are peas, beans, sesame seeds, tuna, milk, and eggs.
Adding probiotics to your diet can help maintain live, helpful bacteria in the gut- preventing serious conditions like chronic diarrhea.
In its raw form, it helps in the optimal functioning of the thyroid gland.
This helps in losing weight, increasing metabolism, and balancing body temperature.
It helps in maintaining a balanced production of hormones in the body.
It helps in removing body toxins and regulate body fat.
A deficiency of vitamin D can lead to thyroid problems.
Ensure that you get at least 15 minutes of sunlight daily for optimal vitamin D production.
Foods that are rich in this vitamin are mackerel, orange juice, egg yolks, and dairy products.
Upload your DNA raw data to Xcode Life for insights into 700+ health-related traits.
